howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Anemia
Introduction:
- Anemia is a condition in which the red cell mass or oxygen carrying capacity is insufficient to meet physiological needs.
- But, as it is difficult is measure, anemia is defined on the basis of hemoglobin content of blood. It is defined as a state in which the blood hemoglobin level is below the lower limit of normal range for the patient’s age and sex.
Age (year) / Sex | Cut off values of hemoglobin (g/dl) |
Both sexes 1 – 1.9 |
11.0 |
2 – 4.9 | 11.2 |
5 – 7.9 | 11.4 |
8 – 11.9 | 11.6 |
Female 12 – 14 |
11.8 |
15 – 17 | 12.0 |
>18 | 12.0 |
Male 12 – 14 |
12.3 |
15 – 17 | 12.6 |
> 18 | 13.6 |
- Situations where hemoglobin concentration may wrongly estimate the oxygen delivery capacity of the blood:
- Acute blood loss
- Compartmental fluid shifts
- Burns
- Pregnancy
- Splenomegaly
- Paraproteinemia.
- Hypoxia
- Living at high attitude
- Respiratory dysfunction
- Cardiac disease
- High affinity Hemoglobins
- Non-functionalhemoglobins
- Alkalosis
- Abnormal blood rheology.
- Decreased red cell flexibility
- Increased nucleated cell count
- Paraproteinemia.
- It is apt to investigate for cause of anemia even if hemoglobin is in normal range in certain conditions, such as
- Hemoglobin is expected to be high as in case of smokers.
- Drop on hemoglobin from previous value but still in normal range.
- Macrocytosis with normal hemoglobin can be due to vitamin B12 deficiency.
- If raw material supply is adequate, production of RBCs can be increased up to 5-10 times the normal. So anemia develops if
- Erythrocyte loss / destruction exceeds maximal capacity of BM, RBC production
- Impaired RBC production within bone marrow.
- Also, a haemoglobin value within the normal range does not necessarily denote the absence of hemolysis.
- While evaluating 2 fundamental questioning should be considered
- What is the cause of anemia?
- What is the urgency for correcting anemia.i.e. whether blood transfusion is needed.
Causes of anemia
- Anemia due to impaired red cell production
- Iron deficiency anemia
- Megaloblastic anemia.
- Anemias due to other nutritional deficiencies- Vitamin A, Pyridoxine, Riboflavin, Niacin, Vitamin C, Vitamin E, Copper, Zinc, Selenium
- Sideroblastic anemia.
- Aplastic anemia and other BM failure disorders
- Bone marrow infiltration: Metastatic bone marrow disease, leukemia, lymphoma, Lipid storage diseases, Military tuberculosis, Fungal infection, osteoporosis, myelofibrosis .
- Anemia of chronic diseases
- Anemia of renal disease
- Anemia of hepatic disease
- Anemia of endocrine disorders- Hypothyroidism, Hypopituitarism, Decreased androgens, Addison’s disease
- Lead toxicity
- Pure red cell aplasia
- Myelodysplastic syndrome
- Congenital dyserythropoietic anemia
- Alcoholism.
- Anemia due to increased RBC destruction (Hemolytic anemia)
- Intra-corpuscular causes:
- Enzymes (Enzymopathies): Glucose 6 phosphate dehydrogenase deficiency, Pyruvate kinase deficiency, 5 nucleotidase deficiency.
- Cell membrane (Membranopathies): Hereditary spherocytosis, Hereditary elliptocytosis, Pyropoikilocytosis, Hereditary stomatocytosis, Hereditary xerocytosis, Paroxysmal nocturnal hemoglobinuria (PNH is the only acquired condition in intra-corpuscular causes)
- Hemoglobin (Hemoglobinopathies)
- Qualitative abnormalities- Occur due to mutations that change amino acid sequence of the globinchain leading to instability or abnormal oxygen transport (due to mutations altering amino acid sequence of globin chain)- Sickle cell anemia, HbC disease, HbD disease, HbE disease, Unstable hemoglobin, Hemoglobin with altered oxygen affinity
- Quantitative abnormalities- Reduced production of one or more globin chains- Alpha thalassemia, Beta thalassemia
- Non transfusion dependent thalassemia- HbE/beta thalassemia, HbC/beta thalassemia, DeletionalHbH disease etc
- Extracorpuscular causes:
- Microangiopathic hemolytic anemia-
- Thrombotic thrombocytopenic purpura
- DIC
- Hemolytic uremic syndrome/ Atypical hemolytic uremic syndrome
- Preeclampsia/ Eclampsia with HELLP syndrome
- Disseminated malignancy
- Associated with malignancy
- Vasculitis- Polyarteritisnodosa, Wagener's granulomatosis, acute glomerulonephritis, Rickettsia like infections
- Systemic lupus erythematosis, scleroderma
- Abnormalities of renal vasculature- Malignant hypertension, acute glomerulonephritis, scleroderma, allograft rejection
- Disseminated intravascular coagulation
- Malignant hypertension
- Catastrophic APLA
- Drugs- Ciclosporine, mitomycin, ticlopidine, clopidogrel, tacrolimus, cocaine
- Systemic infections- Bacterial endocarditis, brucellosis, CMV, HIV, Ehrlichiosis, Rocky mountain spotted fever
- Total body irradiation
- Snake bite
- Physical injury at other sites
- Atrioventricular malformations
- Hemangioendotheliomas
- Giant cavernous hemangiomas (KasabachMeritt syndrome)
- Atrioventricular shunts
- Transjugularintrahepaticportosystemic shunt
- Cardiac abnormalities- Replaced valve, prosthesis, graft, regurgitant jets due to valvular abnormalities
- March hemoglobinuria
- Physical injury to RBCs
- Hypotonic lysis- Drowning
- Pore formation within RBC membrane by Bee/ Wasp sting, spider/scorpion bite
- Cobra bite
- Membrane damage by biotoxins- Bacillus cereus infection, sea cucumber/ sea anemone bites
- Heat induced hemolytic anemia- Extensive burns, use of cell warmers, heat stroke
- Chemical injury to RBCs
- Oxidising agents- Hyperbaric oxygen, arsine gas, chlorates
- Chemicals- Aniline, formaldehyde, hydroxylamine, lysol, mineral spirits, nitrobenzene
- Metals- Lead, copper (Ingestion of copper sulphate, hemodialysis fluid contaminated by copper pipes, Wilson's disease)
- Drugs- Ribavarine, phenazopyridine (urinary bladder analgesic)
- Anemia due to infections
- Direct invasion of RBCs- Malaria, babesia, bartonella
- Production of hemolysins- Cl. Perfingens
- Septicemia/endocarditis by streptococci, staphylococci, salmonella and enterococci. Occurs due to direct toxic effect of bacterial product on RBCs.
- Stimulation of immune response- Mycoplasma, HIV, CMV, EBV
- Enhancing macrophage induced hemophagocytosis- Hemophilusinfluenzae
- Microangiopathichemolytic anemia- Shigella, camphylobacter, aspergillus
- Induction of hypersplenism
- Auto immune hemolytic anemia.
- Mismatched blood transfusion
- Hemolytic disease of new born.
- Hypersplenism.
- Microangiopathic hemolytic anemia-
- Intra-corpuscular causes:
- Anemia due to blood loss
- Acute
- Chronic.
Clinical features: (Depend on degree of anemia, rate at which it has evolved, oxygen demand of the patient, pre-existing comorbidities like IHD)
- Symptoms:
- Fatigue, generalized weakness, lassitude, lethargy
- Breathlessness on exertion
- Palpitation
- Throbbing in head and ears
- Dizziness, tinnitus, headache
- Dimness of vision
- Anorexia, Nausea
- Insomnia
- Paresthesia in fingers and toes
- Angina which may lead to congestive cardiac failure.
- Intermittent claudication
- Transient ischemic attack
- Menstrual disturbance-Amenorrhoea, menorrhagia etc
- Loss of libido
- Signs
- Pallor-observed in skin, conjunctiva, palm, mucus membranes, nail beds etc.
- Due to hyper dynamic state.
- Tachycardia
- Wide pulse pressure with collapsing pulse.
- Mid systolic flow murmur.
- Edema.
- Retinal hemorrhage-Due to increased force in vascular tree.
- In Severe cases: CCF, Angina/MI, Arrythmia
- Additional clinical features in case of hemolytic anemia.
- Jaundice.
- Gall stones
- Dark/Red urine.
- Extra medullary hematopoietic masses-Spleen, liver, lymph node, perinephric tissue.
- Splenomegaly in some cases
- Chronic hemolysis leads to scavenging of nitric oxide by free hemoglobin. This can result in erectile dysfunction, esophageal spasm, renal insufficiency and vascular sequelae such as non-healing skin ulcers and pulmonary hypertension.
Investigation for evaluation of anemia
- Complete hemogram including red cell indices
- Reticulocyte count and reticulocyte production index
- Peripheral smear
- To know type of anemia.
- Basophilic stippling in lead toxicity
- Tear-drop cells in myelofibrosis
- Spherocytes –AIHA, HS.
- Helmet/Schistocytes- MAHA.
- Sickle cells.
- Spur cells-Liver disease.
- Bite cells- G6PD deficiency.
- Agglutination- Cold agglutination disease.
- Increased number of polychromatophilic cells and nRBCs- in hemolytic anemia.
- Blasts/abnormal cells in case of leukemia.
- Hypersegmented neutrophils in megaloblastic anemia.
- WBCs and platelet reduction in case of pancytopenia.
- Parasites can be seen.
- Bone marrow examination-Aspiration and biopsy
- Other tests based on differential diagnosis- Ex: Iron profile, S.B12 estimation etc.
- Investigations in case of suspected hemolytic anemia
- Reticulocyte count- Increased
- Serum bilirubin- Elevated unconjugatedbilirubin (More than 80% of total bilirubin is unconjugated bilirubin)
- Serum LDH level-Raised.
- Serum Haptoglobulin level-Decreased- As haptoglobulin binds to free hemoglobin in plasma and helps in its clearance. Haptoglobulin level is decreased also in case of liver disease, hereditory deficiency.It is increased in case of inflammation as it is an acute phase reactant.
- Similarly hemopexin level is also decreased
- Free hemoglobin in plasma- Raised (Hemoglobinemia).
- Urine- Hemoglobinuria, Hemosiderinuria.
- Further investigations, once presence of hemolysis is confirmed (To know the exact cause of hemolysis)- Tests are chosen based on history, examination and peripheral smear finding.
- Repeat peripheral smear to look for any missing findings
- DCT, ICT
- Osmotic fragility/EMA dye binding test.
- Hemoglobin electrophoresis.(HPLC)
- Test for unstable hemoglobin
- PNH work up.
- HbH preparation
- G6PD screening/Heinz body preparation.
- Genetic tests for thalassemia syndromes.
- Urine for hemoglobin and hemosiderin- They are positive in conditions with intravascular hemolysis, which include:
- Mismatched blood transfusion
- G6PD deficiency
- Red cell fragmentation syndromes (MAHA)- TTP, HUS, DIC, vasculitis, malignant hypertension, HELLP syndrome, Cyclosporine toxicity.
- Some autoimmune hemolytic anemia- IgM related/Compliment mediated.
- Paroxysmal nocturnal hemoglobinuria.
- Paroxysmal cold hemoglobinura
- Some drug induced/infection induced hemolytic anemia.
- March hemoglobinuria.
- Unstable hemoglobin
- Clostridial sepsis
- In case of extravascularhemolysis, RBC destruction occurs within the macrophages of liver and spleen, hence there is no haemoglobinuria or hemosiderinuria
- Targeted Next Generation Sequencing
- Tests multiple candidate genes which are involved in congenital haemolytic anemia.
- This test can be done even in a heavily transfused patient
- Small amount of blood is adequate for carrying out the test
- Genes chosen vary from panel to panel
- Whole genome sequencing is necessary, if targeted NGS fails to identify any genetic abnormality
Pathological changes in various organs due to anemia
- Skin is thin and inelastic due to atrophy of epidermis and dermis.
- Heart- Fatty changes in myocardium
- Kidney- Ischemic necrosis of epithelial cells of proximal convoluted tubule.
- Liver- Centrilobularhepatocyte necrosis.
- Brain- Ischemic necrosis of sensitive ganglion cells of cortex and basal ganglia.
Approach to diagnosis in anemia
Causes of microcytic hypochromic anemia:
- Iron deficiency anemia
- Beta thalassemia major/ trait
- Alpha thalassemia
- Hb E trait/ disease
- Other rare hemoglobinopathies
- Sideroblastic anemia
- Myelodysplastic syndrome
- Anemia of chronic disease
- Lead poisoning
- Hereditaryspherocytosis (Rarely)
Diagnostic algorithm:
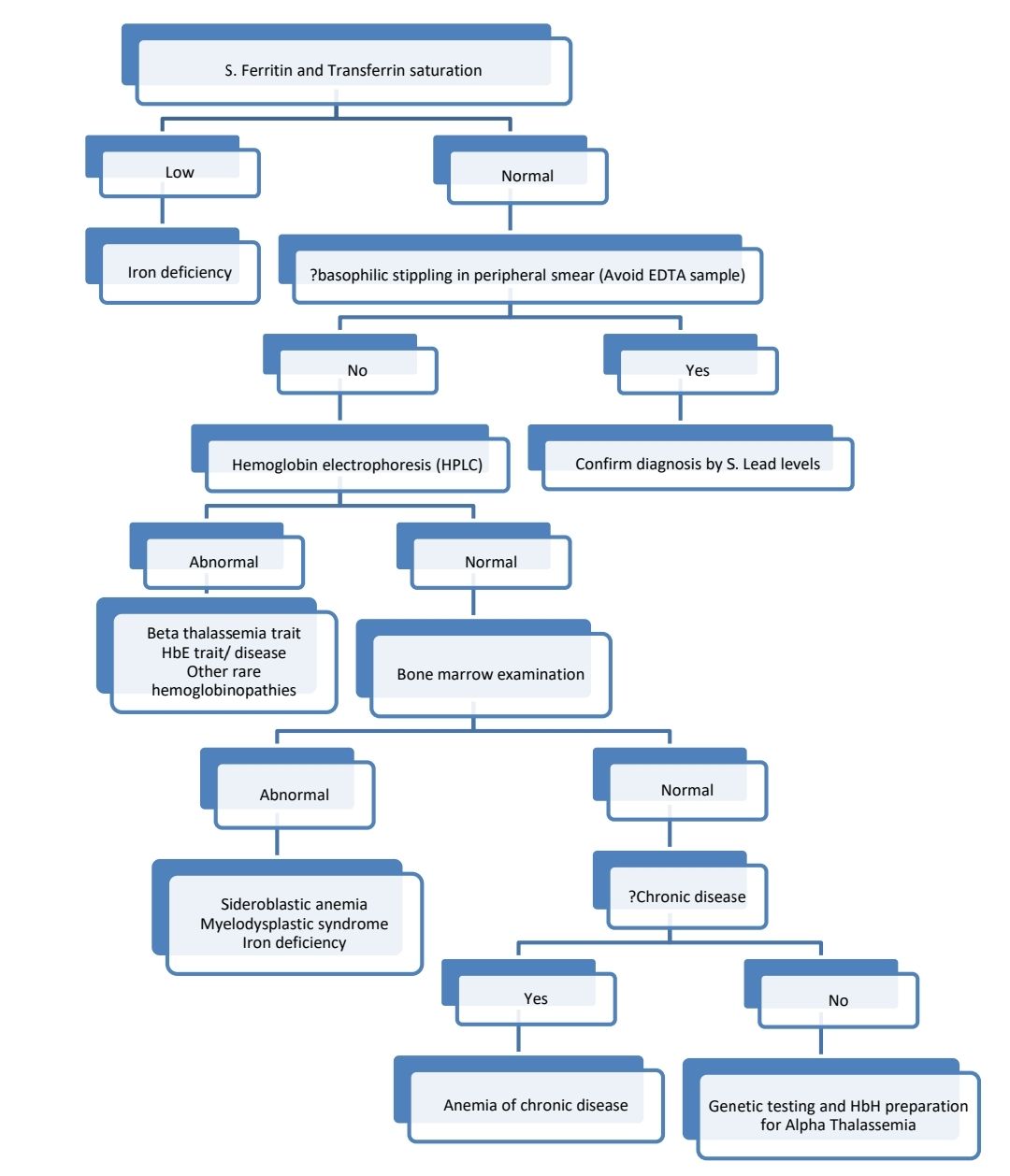
- Transferrin saturation= (S. Iron ÷ TIBC) x 100
- Mentzer Index= MCV ÷ RBC
- <13 is suggestive of thalassemia trait
- >13 is suggestive of iron deficiency
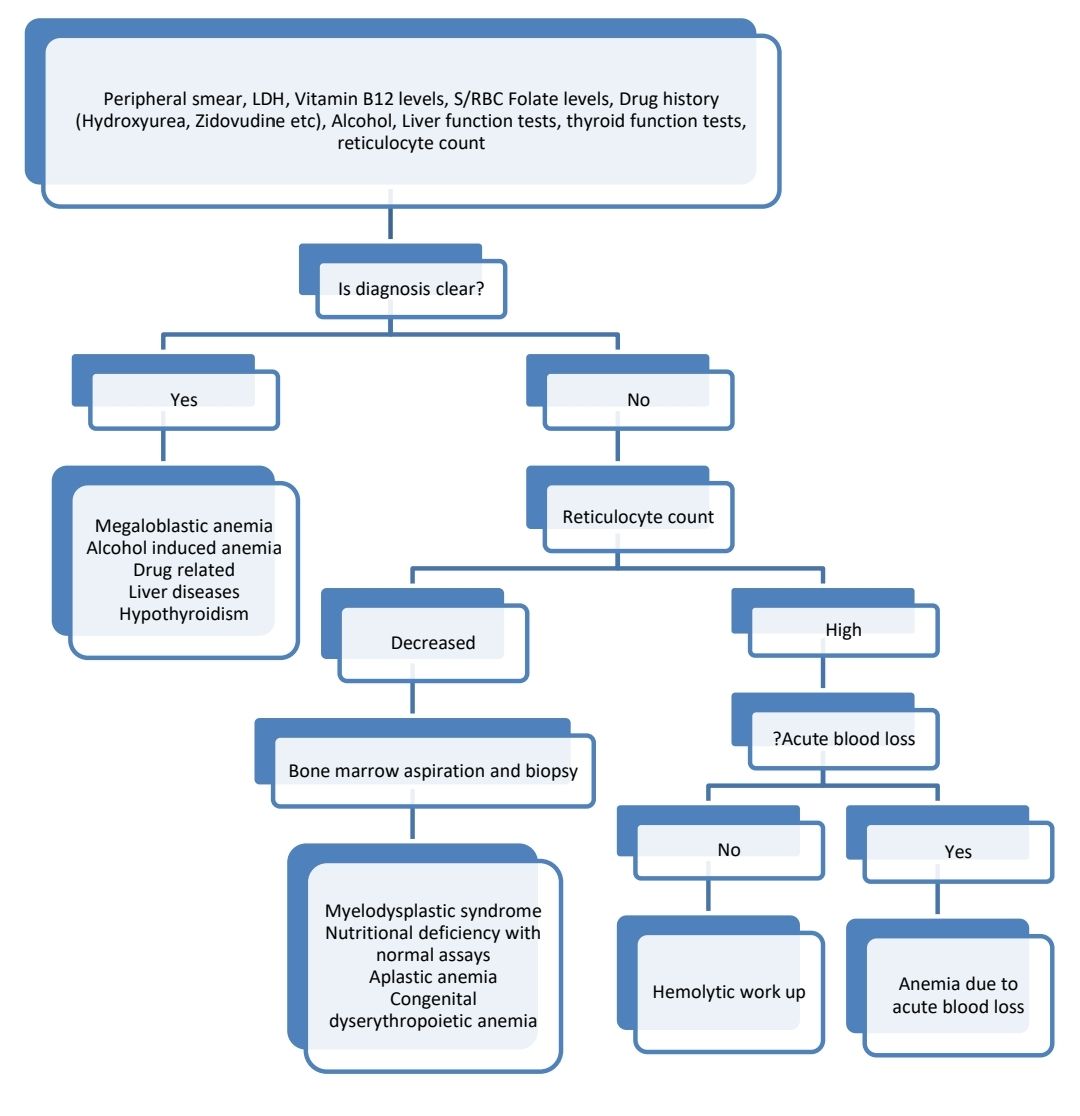
Causes of macrocytic anemia:
- Megaloblastic anemia
- Alcohol induced anemia
- Drug related
- Liver diseases
- Hypothyroidism
- Myelodysplastic syndrome
- Aplastic anemia
- Congenital dyserythropoietic anemia
- Hemolytic anemia
- Anemia due to acute blood loss
Diagnostic algorithm:
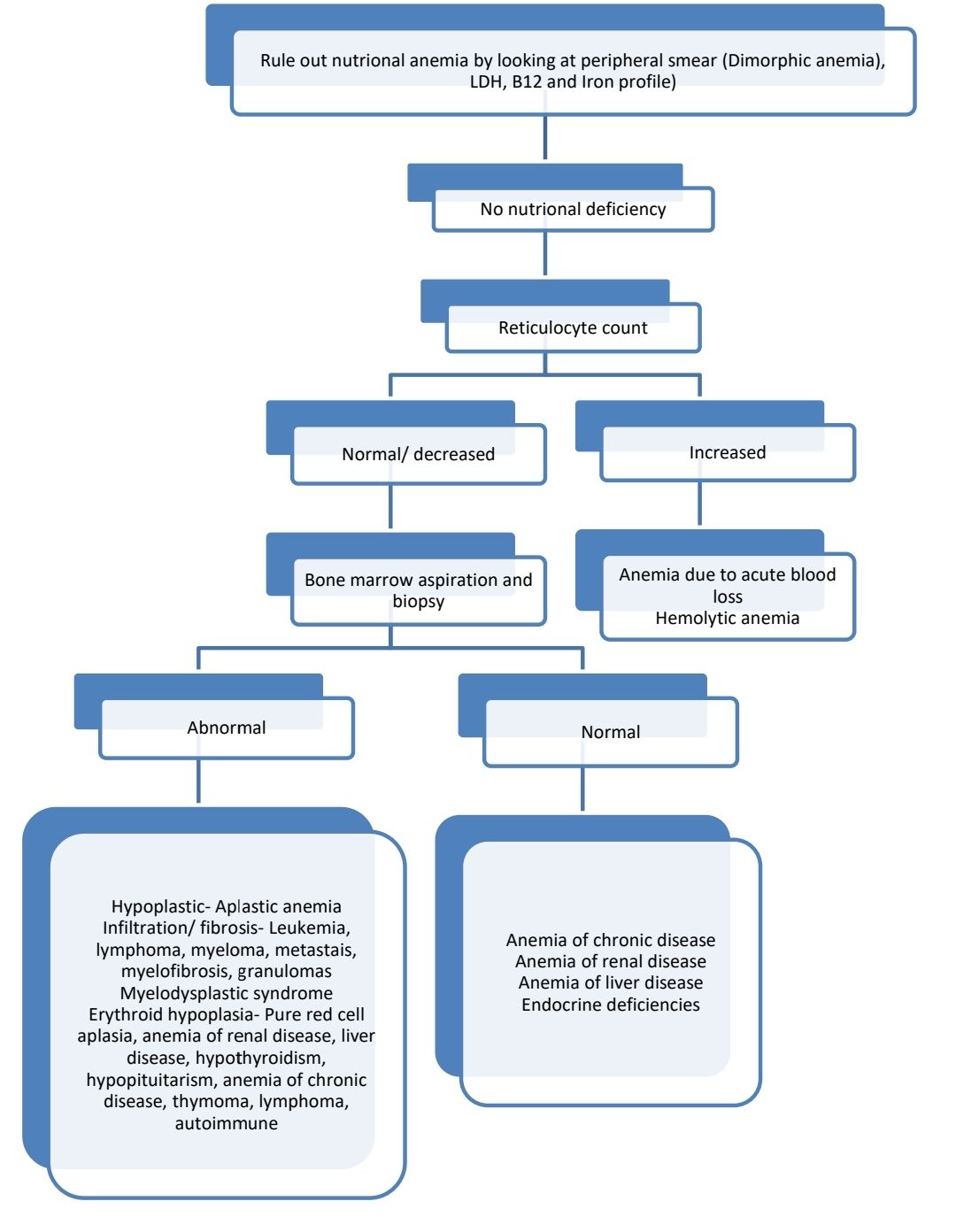
Causes of normocytic normochromic anemia:
- Secondary aplastic anemia
- Idiopathic aplastic anemia
- Bone marrow infiltration- Leukemia, Lymphoma, Myeloma, Metastatic tumor
- Myelodysplastic syndrome
- Pure red cell aplasia
- Anemia of renal disease
- Anemia of liver disease
- Anemia of endocrine origin
- Anemia of chronic disease
- Hemolytic anemia
- Anemia due to acute blood loss
Diagnostic algorithm:
Diagnostic algorithm in case of haemolytic anemia:
(Diagnosis of haemolytic anemia: Low haemoglobin, indirect bilirubin is increased and >80% of total bilirubin, raised reticulocyte count, raised LDH and decreased haptoglobin)
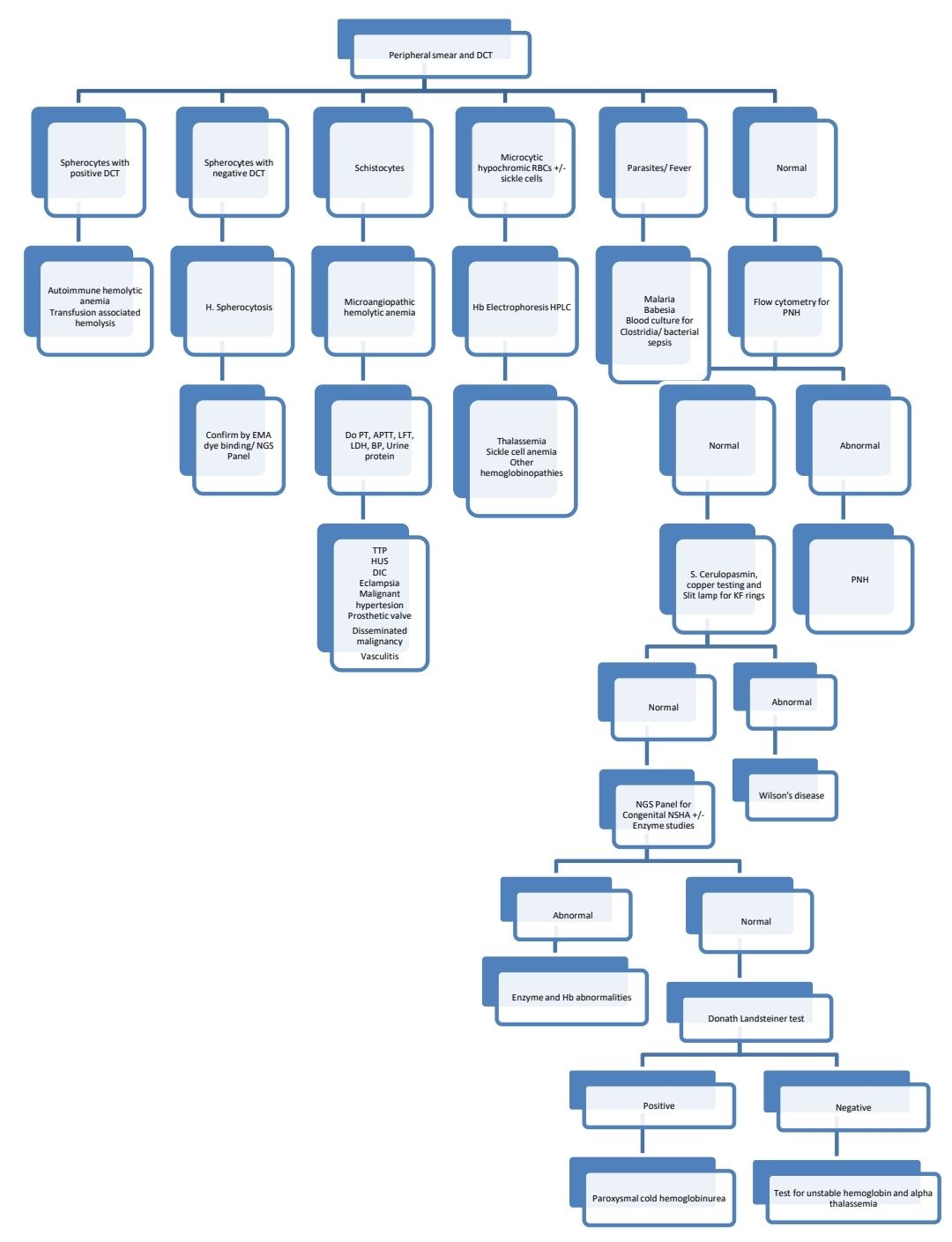
(Rare causes are not part of algorithms. Hence, if unable to get diagnosis by following above algorithms, just go by absolute reticulocyte count and go through entire list of causes of anaemia mentioned above)
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.