howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Disseminated Intravascular Coagulation
Introduction:
- It is an acquired syndrome characterized by the intravascular activation of coagulation with loss of localization arising from different causes. It can originate from and cause severe damage to the microvasculature, which, if sufficiently severe can produce organ dysfunction
Etiology:
- Obstetric complications (Release of tissue factor from damaged fetus/ placenta into circulation): Abruptioplacentae, septic abortion and chorioamnionitis, amniotic fluid embolism, intrauterine fetal death, degenerating hydatidiform moles and leiomyomas, postpartum hemolytic-uremic syndrome, tetracycline – induced hepatorenal failure, fetomaternal blood passage, saline and urea induced abortions, acute fatty liver of pregnancy
- Infections (Endotoxins bind to monocytes via CD14 and bind to endothelial cells via toll like receptors. This leads NF kappa beta activation which results in increased expression of tissue factor and proinflammatory cytokines)
- Viral (herpes, rubella, smallpox, acute hepatitis, Reye syndrome, cytomegalic inclusion disease, various epidemic hemorrhagic fevers, others)
- Rickettsial (Rocky Mountain spotted fever, others)
- Bacterial (meningococcemia, septicaemia, particularly that due to gram negative organisms)
- Mycotic (histoplasmosis, aspergillosis)
- Protozoal (malarial, kala-azar, trypanosomiasis)
- Neoplasms (Express procoagulant molecules like tissue factor, cysteine protease, endopeptidase and mucin)
- Carcinomas (prostate, pancreas, breast, lung, ovary, many others)
- Miscellaneous (metastatic carcinoid, rhabdomyosarcoma, neuroblastoma, others)
- Disorders of the hematopoietic system
- Acute leukemia especially acute promyelocytic leukemia
- Intravascular hemolysis (transfusion of incompatible blood, drug induced, paroxysmal nocturnal hemoglobinuria, sickle cell anemia, fresh-water submersion)
- Vascular disorders- Malformations- giant hemangioma (Kasabach-Merritt syndrome) aneurysms, coarctations of the aorta and other large vessels, Takayasuaortitis, large prosthetic arterial grafts, cyanotic congenital cardiac lesions
- Collagen vascular disorders
- Hypoxia and hypoperfusion- congestive failure with pulmonary emboli myocardial infarction, cardiac arrest, various forms of shock, hypothermia.
- Massive tissue injury- Large traumatic injuries and burns, extensive surgical intervention, extracorporeal circulation, fat embolism
- Miscellaneous- Acute iron toxicity, head trauma, snakebite, anaphylaxis, heat stroke, allograft rejection, graft –versus-host disease, severe respiratory distress syndrome, diabetic acidosis, status epilepticus, acute pancreatitis, homozygous deficiency of protein C.
Pathogenesis:
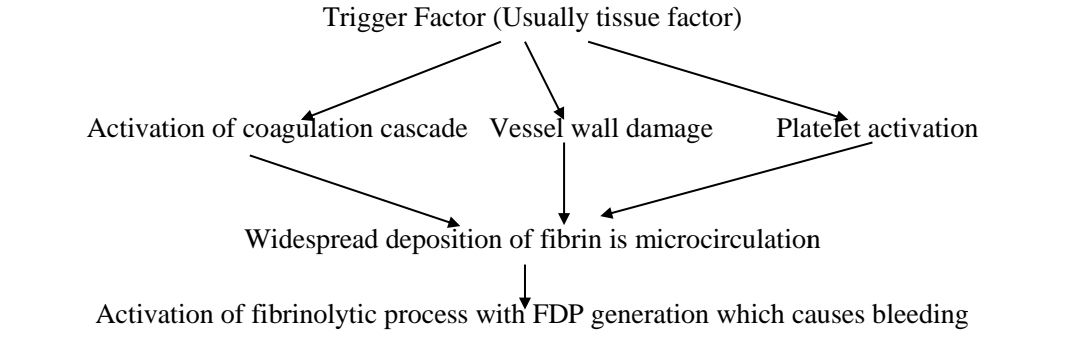
Ischemia of vulnerable organs leading to multi-organ dysfunction
- Fragmentation of RBCs as they squeeze through the narrowed vasculature leading to microangiopathic haemolytic anemia
- Consumption of coagulation factors and platelets leading to generalized bleeding tendency
Subtypes:
- Bleeding type:
- Fibrinolysis is remarkable and dominant
- Seen in APML, obstetric causes, aneurysms
- Organ failure type
- Hypercoagulation is remarkable and dominant
- Seen in sepsis
- Massive bleeding/ consumptive type
- Both are remarkable and strong
- Non-symptomatic
- Both are weak
- Only abnormalities in lab tests are observed
Clinical Features:
- Severity depends on underlying condition
- Bleeding diathesis – mucosal oozing, GI bleed, bleeding from surgical incision and IV lines
- Microangiopathichemolytic anemia
- Reparatory symptoms like dyspnea and cyanosis due to ARDS
- CNS-convulsions, focal lesions, bleeding and coma
- Acute adrenal insufficiency due to adrenal bleed
- Renal – Oliguria, and acute renal failure
- Digital ischemia and gangrene
- Acute liver failure
- Cardiovascular- Shock, acidosis, MI
Investigations:
- Hemogram:
- Hemolytic picture with plenty of schistocytes / fragmented RBCs
- Platelet count-decreased (Measurement of “drop” in platelet count is more important than single time count)
- Prothrombin time – prolonged
- Activated partial thromboplastin time – prolonged
- Thrombin time- prolonged
- Fibrinogen concentration by Clauss method – decreased
- Levels of fibrin degradation products (especially D-dimer) – elevated (Done by ELISA or latex agglutination method)
- Levels of thrombin- Antithrombin complex and prothrombin fragment- 1.2- Elevated. It is the most sensitive test for ongoing activation of coagulation pathway.
- S. Protein C and antithrombin levels- Decreased. It indicates severity of DIC.
- S. Plasminogen and alpha 2 antiplasmin- Decreased
- Levels of soluble fibrin monomers (SFM):
- Reflects thrombin action on fibrinogen
- It is generated only intravascularly, hence its levels are not influenced by local inflammation or trauma.
- Factor 8 levels- Paradoxically increased, probably because of massive release of vWF.
- Thromboelastography
- Diagnostic sensitivity and specificity is unclear
- Biphasic wave pattern with APTT.
Criteria for Diagnosis:
Diagnostic algorithm for the diagnosis of overt DIC
- Does the patient have an underlying disorder known to be associated with DIC? (If yes, proceed; if no, do not use this algorithm)
- Platelet count (> 1lac/cmm = 0; < 1lac/cmm = 1, < 50,000/cmm =2)
- Elevated FDP/SFM (no increase=0; moderate increase=2; strong increase=3)
- Prolonged PT (by < 3 sec=0; > 3sec but < 6 sec = 1; > 6 sec = 2)
- Fibrinogen level (> 1 g/L = 0; < 1g/L =1)
- Score ≥5 compatible with overt DIC
- Score < 5 suggestive (not affirmative) of non overt DIC; repeat tests in 1-2 days.
Differential Diagnosis:
- Sepsis
- Massive blood loss
- Thrombotic microangiopathy
- Heparin induced thrombocytopenia
- Liver disease
- HLH
- Catastrophic APLA
Treatment Plan:
- Vigorously treat underlying condition
- Correct hypotension
- Improve tissue perfusion
- Correct acidosis
- Treatment of hypoxia
- If sepsis- Consider APC infusion
- Consider replacement therapy along with heparin infusion in following cases
- Major thromboembolism
- Purpurafulminans
- Acute promyelocytic leukemia
- Hemangioma
- Aneurysm (before surgery)
- Amniotic fluid embolism
- Septic abortion
- Dead fetus
- For rest of patients: Give only replacement therapy
- Assess every 6-8hrs- clinically and laboratory tests- Give replacement therapy every 8 hrs
- If above fails- consider adding heparin infusion.
About Each Modality of Treatment:
- Replacement therapy:
- Transfusions should not be instituted on the basis of laboratory tests alone
- Indications for transfusions include
- Active bleeding
- Require invasive procedures
- At risk of bleeding complications
- Suggestion that transfusions “add fuel to the fire”, has never been proved in clinical/ experimental studies.
- Components to be administered as replacement therapy include:
- Platelet transfusion – To maintain platelet count more than 20 x 109/L (50 x 109/L if invasive procedures are planned)
- FFP- 15ml/Kg- To maintain PT and APTT - <1.5 x Normal
- Cryoprecipitates- 2bags- Aim should be to maintain fibrinogen of greater than 1 g/L
- Packed RBCs- To maintain haemoglobin >9gm/dl
- Heparin infusion
- 500-750 units / hour (Low dose unfractionated heparin)
- Maintain APTT to 1.5 to 2.5 times the normal
- Should be continued till underlying disease responds to the treatment
- LMWH can be used in place of UFH- It should be given in prophylactic doses.
- Efficiency of heparin therapy is monitored by
- Serial platelet counts
- FDP quantification
- Fibrinogen levels
- Heparin should not be used in DIC caused by
- Placental abruption
- Sepsis
- Severe liver disease
- Major trauma
- Activated Protein C concentrates
- Dose- 24microgm/Kg per hour as continuous infusion
- Useful in sepsis induced DIC
- Partially effect is due to anti-inflammatory effect
- Some studies have shown that there is no use of APC
- Important points to note
- Never use antifibrinolytic agents, as it aggravates tissue ischemia and causes severe thrombosis
- Exceptions to this include: APML, giant hemangioma, amniotic fluid embolism, metastatic prostatic carcinoma. They may be used if patient is profusely bleeding in spite of adequate replacement therapy.
Other Treatment Options:
- Tissue factor inhibitors
- Recombinant TFPI - Inhibits TF activity
- Monoclonal antibodies- Inhibit TF activity ; binds to endotoxin
- Inactivated factor VIIa
- Rec Human soluble thrombomodulin
- Synthetic protease inhibitors: Ex: Gabexatemesilate and nafamostat
Related Disorders:
- Chronic form of DIC is seen with
- Malignancy – Especially mucin secreting adenocarcinoma
- Aortic aneurysm
- Vascular malformation
- Retained dead fetus syndrome
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.