howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Febrile Neutropenia
Introduction:
- Febrile neutropenia is defined as a single oral temperature of >380 C or 1000 F for more than 1hr in a patient with absolute neutrophil count of <500/cmm or <1000/cmm which is expected to decrease to <500/cmm in next 48hrs.
- Avoid axillary temperature as it does not reflect core body temperature.
- Avoid rectal temperature as colonizing gut organisms may enter surrounding mucosa and soft tissue.
- Most of the standard chemotherapy regimens have 6-8 days of neutropenia.
- For causes of neutropenia, refer to “Approach to diagnosis” section.
- For Congenital and other neutropenias, refer to “Miscellaneous diseases” section.
- ANC = TLC x percentage of neutrophils ÷ 100
- High-risk patients:
- Expected neutropenia for >7 days
- Significant hepatic or renal or respiratory dysfunction
- Signs of severe sepsis or septic shock:
- Hemodynamic instability
- Mental status changes of new onset
- Respiratory dysfunction
- Oliguria
- Oral or gastrointestinal mucositis
- Intravascular catheter infection
- New pulmonary infiltrate or hypoxemia
- Complex infection at the time of presentation
- Uncontrolled or progressive cancer
Common pathogens
- Bacteria
- Gram Negative Bacilli:
- Klebsiella, E. Coli, Pseudomonas, Proteus, Citrobacter, Acinetobacter, Stenotrophomonas maltophilia
- They cause pneumonia, soft tissue infection, perirectal infections, primary bacteremia
- Gram Positive Cocci:
- Staphylococcus, Enterococcus, Streptococcus virudans
- They cause line related infections
- Anaerobes
- They cause periodontal infections
- Encapsulated organisms (Hemophilus, Pneumococcus)
- They cause infections in patients with Hodgkin's disease, NHL and CLL
- Gram Negative Bacilli:
- Fungi
- Candida (Most common fungi), Aspergillus, Cryptococcus, Phycomycetes
- Cause sinus and broncho pulmonary infections
- Viruses
- HSV, VZV, CMV, Adeno, RSV
- Protozoa
- Pneumocystis jiroveci, Toxoplasma Gondi, Strongyloidis stercolaris
- Mycobacteria
Pathogenesis:
- Mucosa is breached due to effect of chemotherapy
- Seedling of bloodstream occurs from the endogenous flora
- Lack of adequate immunity (neutropenia, immune defects due to malignancy and immunosuppressants) further enhances spread of infection.
Types of neutropenic fever syndromes:
- Microbiologically documented infection – Has clinical focus of infection and an associated pathogen
- Clinically documented infection – Has a clinical focus (eg, cellulitis, pneumonia) but without the isolation of an associated pathogen
- Unexplained fever – Has neither a clinical focus of infection nor an identified pathogen
Diagnosis and evaluation:
- Instead of fever, serious infections in neutropenia, can present with
- Hypothermia
- Declining mental status
- Myalgia
- Lethargy
- Local signs of infections like pus formation, induration, erythema or warmth may be absent
- No discernible infiltrate may be noted on chest X ray
- No CSF pleocytosis even in setting of meningitis
- No pus cells in case of UTI
- Should try to rule out following with the help of history, examination and investigations:
- Pneumonia
- Meningitis or encephalitis,
- Enterocolitis
- Urinary tract infections
- Skin and soft tissue infections, including insertion sites of central venous catheters
- Perianal abscess
- History:
- Site specific symptoms: Cough, shortness of breath, sore throat, ear pain, sinus pain, headache, abdominal pain, diarrhea, rashes, dysuria, headache
- Antimicrobial prophylaxis
- Comorbidities
- Infection exposure
- Prior infections and medications
- Examination:
- Oral cavity: Periodontal disease, oral thrush
- Ulcers/ necrotizing lesions involving : gingiva, buccal mucosa, pharynx etc
- Bone marrow aspiration site
- Perianal redness/ tenderness
- Line tenderness
- Systemic examination based on symptoms
- Fever, tachycardia, tachypnea and hypotension
- Investigations
- Complete hemogram
- RFT including electrolytes
- LFT
- CRP, ESR
- Blood culture
- Should be sent prior to starting antibiotic
- Preferably paired culture from PICC/CVC line and peripheral vein
- Minimum 20ml of blood divided into aerobic and anaerobic culture. In pediatric patients (<40kg) proportionately, less volume of blood has to be sent. 1% of total blood volume. (Blood volume= 70ml x Weight in Kg)
- Retain specimen in lab for 10 days as there can be growth of fungi
- If fever persists after starting empirical antibiotic, then 1 more set of blood culture to be sent on each of the next 2 days.
- After initial defervescence occurs with initial antibiotics any recrudescence fever must be evaluated with 1 more set of blood culture.
- 2 blood cultures detect 80-90% of blood stream infections
- Depending on clinical symptoms and signs
- Urine routine and culture
- Sputum/ BAL culture and viral panel
- Stool routine and culture
- Stool for clostridium defficile if patient has loose motions
- CSF routine and culture
- Skin aspiration culture. Suspicious skin lesions to be biopsied
- S. Galactomannan: If aspergillosis is suspected
- Chest X Ray
- CT Thorax (If chest X ray is normal)
- Interstitial infiltrates: D/D Include pulmonary edema, diffuse alveolar damage, idiopathic pneumonia syndrome, respiratory viruses (RSV, Influenza, Para influenza, Adenovirus, Enterovirus, Herpes simplex, CMV, Varicella Zoster, HHV 6), Pneumocystis pneumonia
- Focal air space disease: Bacterial pneumonia, Fungal pneumonia
- Nodules: Fungal pneumonia (Aspergillosis), Nocardia, Legionella, Septic bacterial emboli, Mycobacterial infection with cavitation, EBV Lymphoproliferative disorder, Relapsed malignancy, Pulmonary embolism (Pleural based)
- Halo/ Air crescent sign: Aspergillosis
- Bronchoscopy (If any finding in CT thorax) and BAL for cytology, fungal stain, bacterial stain and aerobic culture, mycobacterial stain and culture, Nocardia culture, Legionella culture, Viral culture, Test for CMV, RSV, Multiplex viral PCR)
- VATS assisted lung biopsy/ CT Guided FNAC- For peripheral lung nodule
- CT Abdomen- For neutropenicenterocolitis
- CT sinuses- For invasive fungal infections
- CT/MRI of brain and CSF analysis- If CNS Symptoms
- Look for non-infectious causes of fever
- Drug related
- Thrombophlebitis
- Underlying cancer
- Resorption of blood from large hematoma
- During treatment:
- CBC, Creatinine, K- Every 3 days: Helps to plan supportive therapy and monitor possible occurrence of drug toxicity
- Transaminases and Bilirubin- Every week
- Repeat imaging as required
- Routine testing of CRP, IL-6, IL-8, Procalcitonin is not recommended
Prognosis:
- Overall in hospital mortality- 10%
- Mortality with proven gram negative bacteremia- 18%
- Mortality with proven gram positive bacteremia- 5%
- Adverse prognostic markers include: Age >65 years, ANC- <100/cmm, Severe infection (Septic shock) and pre-existing comorbidities.
Approaches in management:
- Primary prophylaxis: Administration of an antimicrobial drug to prevent infection in patients at increased risk.
- Secondary prophylaxis: Administration of prophylactic doses of an antimicrobial drug to prevent recurrent infection.
- Empiric therapy: Initiation of therapy at the time of the onset of neutropenic fever without a firm diagnosis of infection.
- Pre-emptive therapy: Initiation of therapy based upon screening with a sensitive microbiology assay (eg, antigen detection or molecular assays).
Prevention:
- Hand hygiene- Wash with soap and water and use sanitizer frequently. This should be done by patients, health workers and patient’s care takers.
- Brush twice daily
- Rinse with sodabicarb/ chlorhexidine thrice a day
- Standard barrier precautions
- Personal hygiene: Daily shower, females must wipe from front to back, do not use tampons
- Treat skin infection and abrasions promptly.
- Avoid contact with flowers, plants, pet animals
- Low bacteria diet: Well cooked food, well cleaned raw fruits and vegetables are acceptable
- Stool softeners to prevent constipation.
- Avoid lactobacillus
- Avoid instrumentation, rectal thermometers, enema, suppository, PR examinations
- Protective isolation and HEPA (High Efficiency Particulate Air) filters for high risk patients. Should remove particle of size of >0.2micrometer diameter. Should have minimum of 12 air exchanges per hour.
- Avoid visitors who are currently symptomatic with infection
- Avoid crowded places
- Visitors should wash hands. Wear gowns.
- Close contacts must be vaccinated against Influenza, mumps, measles, rubella and varicella
- Cotrimoxazole/ Dapsone/ Pentamidine (Aerosolized/ IV) for PCP- Continue for 6 months after completion of therapy. Cotrimoxazole is useful in preventing bacterial infections as well to some extent.
- Acyclovir- 400mg- BD or Valacyclovir- 500mg- BD- for HSV and VZV
- Valganciclovir for CMV (Used in post transplant patients)
- Prophylactic antibiotics in high-risk (ANC <500/cmm for >7 days) patients- Quinolones (Levofloxacin-500mg OD or Ciprofloxacin- 500mg- BD). If giving along with Voriconazole, monitor QTc.
- Fungal
- Use of Fluconazole may increase the growth of other pathogenic fungi. Consider use of fluconazole in patients on high dose steroids.
- For high risk patients use Voriconazole/ Itraconazole/ Posaconazole
- For HBsAg positive patients/ patients with antibody against hepatitis B core antigen, to prevent fulminant hepatitis.
- Entecavir, Tenofovir, Lamivudine
- To be continued for 6-12 months following completion of treatment
- Prophylactic G-CSF/ Peg-G-CSF (6mg- One dose per cycle) in high risk patients
- Vaccinations- Patients and also Health care workers and people coming in contact with patient- must receive yearly Influenza vaccination with inactivated vaccine. Vaccine must be given at least 2 weeks prior to chemotherapy. As postexposure prophylaxis Oseltamivir- 75mg- OD- for 10 days should be given.
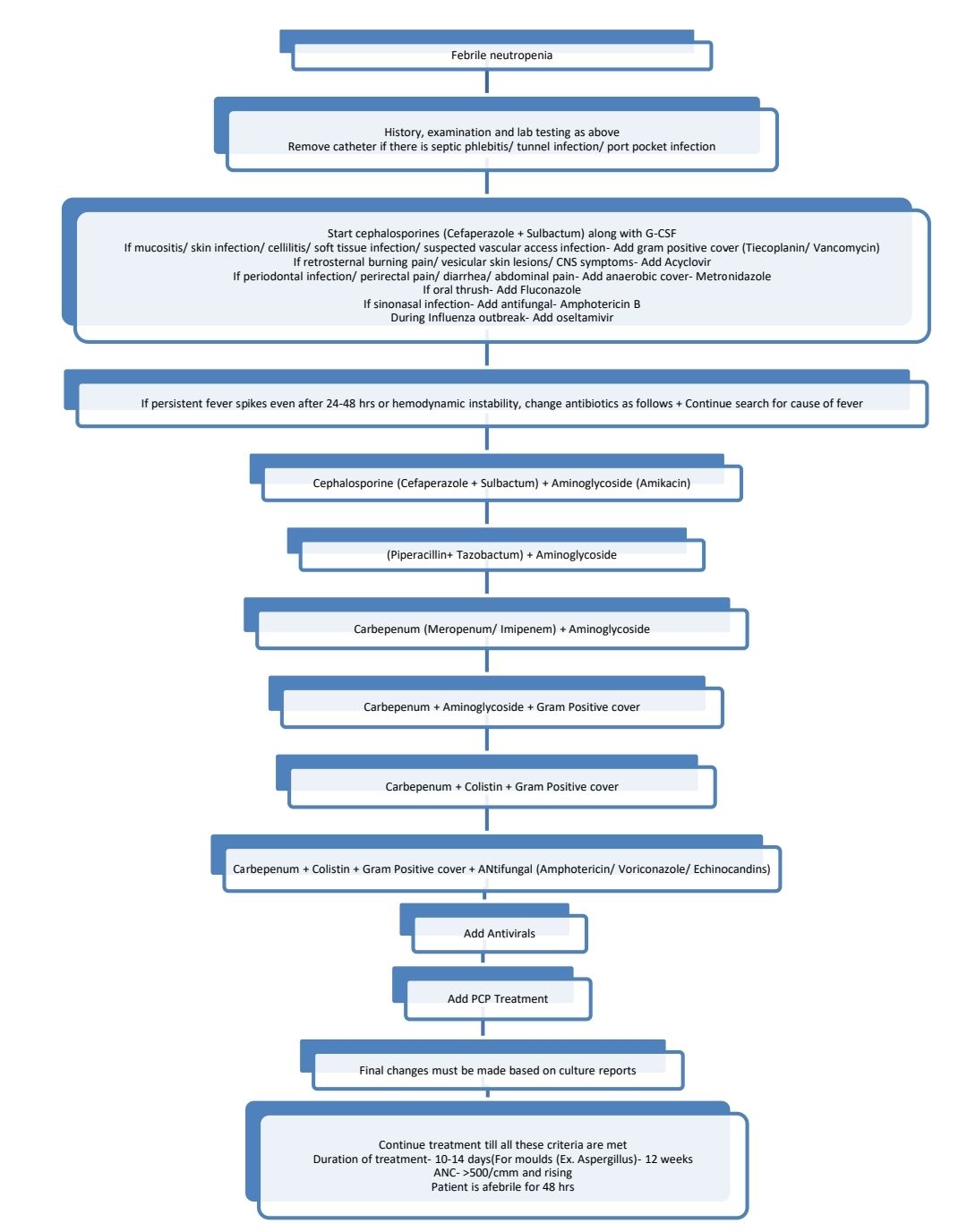
Treatment Plan:
- Start treatment within 1 hr (Antibiotics and G-CSF) after sending investigations and without waiting for reports. Continue all preventive measures.
- Patient can die because of gram negative sepsis within hours after first fever.
(Choice of antibiotics depends on local epidemiological bacterial isolate and resistance patterns)
Anti-microbials active against different organisms
- MRSA (60% of staphylococcus are MRSA): Vancomycin, Teicoplanin, Tigecycline, Daptomycin, Linezolid
- VRE (Vancomycin resistant enterococci): Linezolid, Daptomycin, Tigecycline
- ESBL (Extended spectrum beta lactamase) producing gram negative bacilli: Carbapenems
- KPC (Klebsiella pneumoniae carbapenase): Colistin, Tigecycline, High dose meropenem (6gm/day)
- MDR Pseudomonas: Piperacillin+ Tazobactam + Colistin
- MDR Acinetobacter Baumenii: Colistin+ Rifampin, Tigecycline+ Colistin
- Stenotrophomonas maltophilia: Trimethoprim+ Sulfamethoxazole, Quinolone, Tigecycline
- Cl. difficile- Oral vancomycin/ metronidazole
- Candida (Except C. Gabrata, C. Krusei)
- Stable patient: Fluconazole
- Unstable patient: Echinocandins
- Moulds (Aspergillus fusarium/ Mucor)- Amphotericin, Posaconazole, Echinocandins (Note: Voriconazole does not act against mucor)
- Fusarium, Scedosporium, Pseudollescheria, Trichosporon: Voriconazole, Posaconazole
- HSV, VZV: Acyclovir, Famciclovir, Valacyclovir
- CMV: Ganciclovir, Valganciclovir, Foscarnet
- RSV: Ribavirin
- PCP: Cotrimoxazole, Pentamidine
Note:
- Consider granulocyte infusion if there is invasive fungal infection, GNB sepsis unresponsive to antibiotics
- Single blood culture positive for coagulase negative staphylococcus should generally be dismissed as attributable to a contaminant
- If fever persists after recovery of neutrophils consider hepatospleniccandidiasis, indwelling catheter infection
Causes of fever (Defining fever- >98.960 F at 6am, >99.860 F at 4pm)
- Specific infections
- Viral: Infectious mononucleosis, Dengue, HIV, Chicken pox, Varicella zoster, Erythema infectiousum, Influenza, Measles, Mumps, Rubella. HSV, CMV
- Bacterial: Typhoid, Typhus, Legionnaire's disease, Psittacosis, Syphilis, Brucellosis, Tuberculosis, Tularemia, Gonorrhea, Leptospirosis, Bacteremia (Staphylococcal, Streptococcal, Meningococcal), Rickettsial fever
- Parasites: Malaria, Filaria, Trypanosomiasis, Kala azar,
- Fungal: Aspergillosis, Mucormycosis, Candidiasis, Coccidioidomycosis, Histoplasmosis
- Localized infections: Endocarditis, Prostatic abscess, Ischiorectal abscess, Pyosalpinx, Parametrititis, Sinusitis, Tonsillitis, Osteomyelitis, Suppurative Lymphadenitis, Breast abscess, Empyema, Lung abscess, Liver abscess, Renal abscess, Splenic abscess, Empyema of gall bladder, Suppurative cholangitis, Subdiaphragmatic abscess, Bronchiectasis, Appendicular abscess, Perinephric abscess, Retroperitoneal abscess, Psoas abscess, UTI, Cholecystitis, Thyroiditis, Pneumonia, Colitis, Pancreatitis, Hepatitis, meningitis, encephalitis
- Inflammatory conditions: Ulcerative colitis, Crohn disease, Familial Mediterranean fever, Sarcoidosis
- Connective tissue disorders: SLE, Rheumatoid arthritis, Polymyositis dermatositis, Vasculitis
- Malignancies: Lymphoma, ALL, RCC, Sarcoma
- Allergic reactions: Anaphylaxis, allergic skin rashes, transfusion related fever
- Drug reactions: Sulpha drugs, antibiotics (beta lactums, Dapsone, Allopurinol), iodides, barbiturates, phenytoin
- Others: Pontine hemorrhage, thyrotoxicosis, Heat stroke, Extravasation of blood into tissue space, Venous thrombosis
Definition of Pyrexia of Unknown Origin:
- Fever >1010 F on several occasions
- Duration >3 weeks
- Failure to reach a diagnosis after 1 week of in-patient investigations
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.