howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Follicular Lymphoma
Introduction:
- It is a chronic, relapsing, indolent neoplasm of germinal centre B-cells (centrocytes / cleaved follicle centre cells and centroblasts / Non cleaved follicle centre cells), which has atleast a partially follicular pattern.
- 85% cases harbour t(14;18) translocation
Epidemiology:
- Accounts for 35% of adult NHL
- Median age- 60-65 years
- Slight female predominance
- 85% have advanced disease at presentation
Etiology:
- Agricultural exposure to malathione and DDT
- Cigarette smoking in females
- Spray painters
- Hepatitis C virus infection
- Sjögren’s syndrome
Pathogenesis: Multi-hit lymphomagenesis
t(14;18) translocation with rearrangement involving the IGH and BCL2 genes
↓
Constitutive expression of BCL2
↓
t(14;18) positive memory like B cell clones, which circulate in blood
↓
Repeated germinal center transits with accumulation of oncogenic hits (such as KMT2D and CREBBP mutations)
↓
Evolution of oncogenic variants (Sub-clones) of follicular lymphoma cells
- BCL6 alterations are seen due to rearrangements affecting chromosomal band 3q27 (Seen in 20% cases with BCL2 rearrangement and 35% cases without BCL2 rearrangement)
- 10-15% FL cases do not have BCL2 or BCL6 rearrangements. They have mutations of STAT6 or KMT2D gene.
Classification: 2 types on gene expression profiling:
- Immune response 1 type- Associated with good prognosis
- Immune response 2 type- Associated with poor prognosis
Clinical Features:
- Asymptomatic
- Lymphadenopathy
- Splenomegaly
- B Symptoms
- Fatigue
- Local mass effect due to lymph node enlargement
- Bone marrow failure
Investigations:
- Lymph node biopsy
- Replacement of normal architecture by closely packed neoplastic follicles.
- Neoplastic follicles are
- Poorly defined
- Lack mantle zones
- Closely packed
- Efface the nodal architecture
- Lack tangible body macrophages
- Germinal center shows monomorphic population of cells
- Interfollicular component- Usually small centrocytes and can show phenotypic differences from the cells within the neoplastic follicles
- At places diffuse arrangement seen
- Architectural patterns of follicular lymphoma
- Follicular- Follicles >75%
- Follicular and diffuse- 25-75% follicular
- Focally follicular- <25% follicles
- Diffuse- 0% follicles (Note: it is not same as DLBCL)
- Two types of cells are present
- Centrocytes – Small to medium sized cells. Nuclei are angulated / elongated / twisted / cleaved and have inconspicuous nucleoli. Cytoplasm is scant & pale.
- Centroblasts –They are large transformed cells. Nuclei are indented, hyperchromatic with vesicular chromatin and 1-3 peripheral nucleoli. There is narrow rim of cytoplasm.
- Non neoplastic dentritic follicular cells also may be seen. In contrast to their counterparts in benign follicles, these show no immuno reactivity to Fascin.
- Variations in morphology
- Fine or coarse bands of fibrosis
- Presence of monocytoid B cell / marginal zone differentiation
- Deposition of proteinaceous material in the centre of the nodules- Amorphous, acellular, brightly eosinophilic, and PAS positive
- Presence of large cytoplasmic eosinophilic globules
- Clear-cut plasmacytic differentiation
- Presence of cells with cerebriform nuclei
- Permeation of the tumor follicles by small round lymphocytes of presumably mantle zone origin
- Presence of rosettes
- Presence of hyaline vascular follicles
- Prominent epitheloid granulomatous response
- Grading: Based on centroblasts per HPF (40x) (counted in 10 neoplastic follicles)
- Grade 1 - 0-5
- Grade 2 - 6-15
- Grade 3 - > 15
- 3A- Centrocytes are present
- 3B- Solid sheets of centroblasts
- Peripheral smear: 15% cases show circulating tumor cells
- Very small lymphocytes with no visible cytoplasm
- Nuclear chromatin is smooth without clumps of heterochromatin and no visible nucleoli
- Nuclear shape is angular with a small cleft (Cleaved cells/ buttock cells)
- Bone marrow aspiration and biopsy
- Involved in 50% of cases at presentation
- Paratrabecular distribution
- Follicular pattern
- LDH
- Beta 2 microglobulin
- Flow cytometry on blood or bone marrow or IHC on lymph node biopsy (Immunophenotyping)
- Positive – SIg mostly IgM, Germinal center associatedmarkers (CD10, BCL6, GCET1, HGAL (GCET2), LMO2, AID, MEF2B, and Stathmin), B-cell associated antigens (CD19, CD20, CD22, CD79a, PAX5), CD38, BOB1, BCL2 (BCL2 is absent in normal germinal center cells)
- Some lack CD10, BCL2. BCL2 negative tumors are aggressive
- Negative – CD5, CD43, CD11c, CD25, CD30, CD103, CD138, BCL1, CCND1, IRF4 (MUM1)
- Variable- CD23
- Light chain restriction
- Molecular studies:
- Rearrangement of immunoglobulin heavy and light chain genes
- Somatic mutations in variable region genes. (consistent with derivation from follicle centre cells)
- Cytogenetics:/ FISH:
- t(14;18)(q32;q21)- Results in relocation of BCL-2 anti-apoptosis gene adjacent to an immunoglobulin promoter, leading to over-expression of BCL2 protein.
- +7, +18, 3q27-28, 6q23-26, 17p abnormalities
- Imaging (PET-CT or CT with oral and IV contrast- Neck, chest, abdomen and pelvis): Needed for
- Assessment of disease extent (staging)
- Identifying sites of bulky disease
- To identify the site of biopsy
- Helps in monitoring of patients
- MRI- To be done if there is suspicion of CNS involvement
Criteria for diagnosis:
Essential:
- B-cell lymphoma composed of varying proportions of centrocytes and/or centroblasts/large transformed cells, with the dominance of centrocytes in the overwhelming majority of cases.
- Immunophenotype compatible with germinal center B-cell origin with positivity to markers such as CD10, BCL6, MEF2B, GCET1, GCET2 or LMO2
Desirable:
- At least partly follicular growth pattern
- BCL2 or BCL6 rearrangements and/or lack of IRF4 rearrangement (in equivocal cases)
Prognosis:
- Incurable disease, except in few patients with early stage disease
- 20-30% patients die of disease due to refractory disease or following transformation to high grade lymphoma.
- Median survival- 93 months.
- Indolent course
- Poor prognostic markers are
- Bone marrow involvement
- High beta 2 microglobulin levels
- Grade 3 lesion
- Monocytoid B-cell differentiation
- Presence of more than 6 chromosomal breaks
- Breaks at 6q23-26 or 17p or -1p or +12 or -18p or -1p
- Elderly patients
- Transformation to a large B-cell lymphoma or ALL
- Double hit BCL2 and MYC rearrangements
- Follicular lymphoma International Prognostic Index (FLIPI)- 1 scoring:
- Age >60years
- Ann Abror stage- III or IV
- Hemoglobin- <12gm/dL
- Raised S. LDH level
- Nodal sites >4
- FLIPI- 2 Scoring
- High beta 2 microglobulin
- Bone marrow involvement
- Hemoglobin- <12gm/dL
- Largest diameter of lymph node- >6cm
- Age >60years
- Outcome by FLIPI 1 Scoring
Risk | Number of factors | 5 year OS |
Low | 0-1 | 91% |
Intermediate | 2 | 78% |
High | 3 or more | 53% |
- Outcome by FLIPI 2 Scoring
Risk | Number of factors | Alive at 5 years | PFS | OS |
Low | 0 | 98% | 76% | 96% |
Intermediate | 1-2 | 62% | 46% | 80% |
High | 3-5 | 20% | 29% | 59% |
Indications for Treatment (GELF Criteria):
- 3 or more distinct nodal sites each more than 3cm
- Single nodal site more than 7cm
- Symptomatic splenomegaly
- Cytopenias secondary to lymphoma (Hemoglobin <10gm/dL, TLC <1000/cmm or Platelets <1lac/cmm)
- Circulating lymphoma cells >5000/cmm
- Pleural effusion/ ascitis
- B symptoms
- Threatened end organ damage
- Elevated LDH or beta 2 microglobulin (>3gm/dL)
- Steady/ rapid progression
(Some recent studies indicate that, in case of advanced disease with no indication for treatment, weekly Rituximab for 4 weeks, is safe and cost effective therapy. This approach improved quality of life but not overall survival. Although “no therapy” is the standard of care, Rituximabmonotherapy may also be considered)
Pretreatment Work-up:
- History
- B-Symptoms
- Examination
- LN:
- Spleen:
- WHO P. S.
- BSA
- IHC/Flow cytometry
- Grade
- BMA and Bx
- CT (CAP)/ PET
- Stage
- Hemoglobin
- TLC, DLC
- Platelet count
- LFT: Bili- T/D SGPT: SGOT: Albumin: Globulin:
- Creatinine
- Electrolytes: Na: K: Ca: Mg: PO4:
- Uric acid:
- LDH
- β2 microglobulin
- HIV:
- HBsAg:
- HCV:
- UPT
- Cytogenetics
- FLIPI -1Score
- FLIPI- 2 score
- ECHO (If anthracyclines planned)- LVEF- %
- Chemotherapy consent after informing about disease, prognosis, cost of therapy, side effects, hygiene, food and contraception
- Fertility preservation
- PICC line insertion and Chest X ray after line insertion
- Tumor board meeting and decision
- Attach supportive care drug sheet
- Inform primary care physician
Treatment Plan:
- Limited disease- Stage I or Stage II (Contiguous)
- ISRT- Then assess response
- CR/PR- Follow up- If progression of disease treat as extensive disease
- NR- Treat as extensive disease
- ISRT- Then assess response
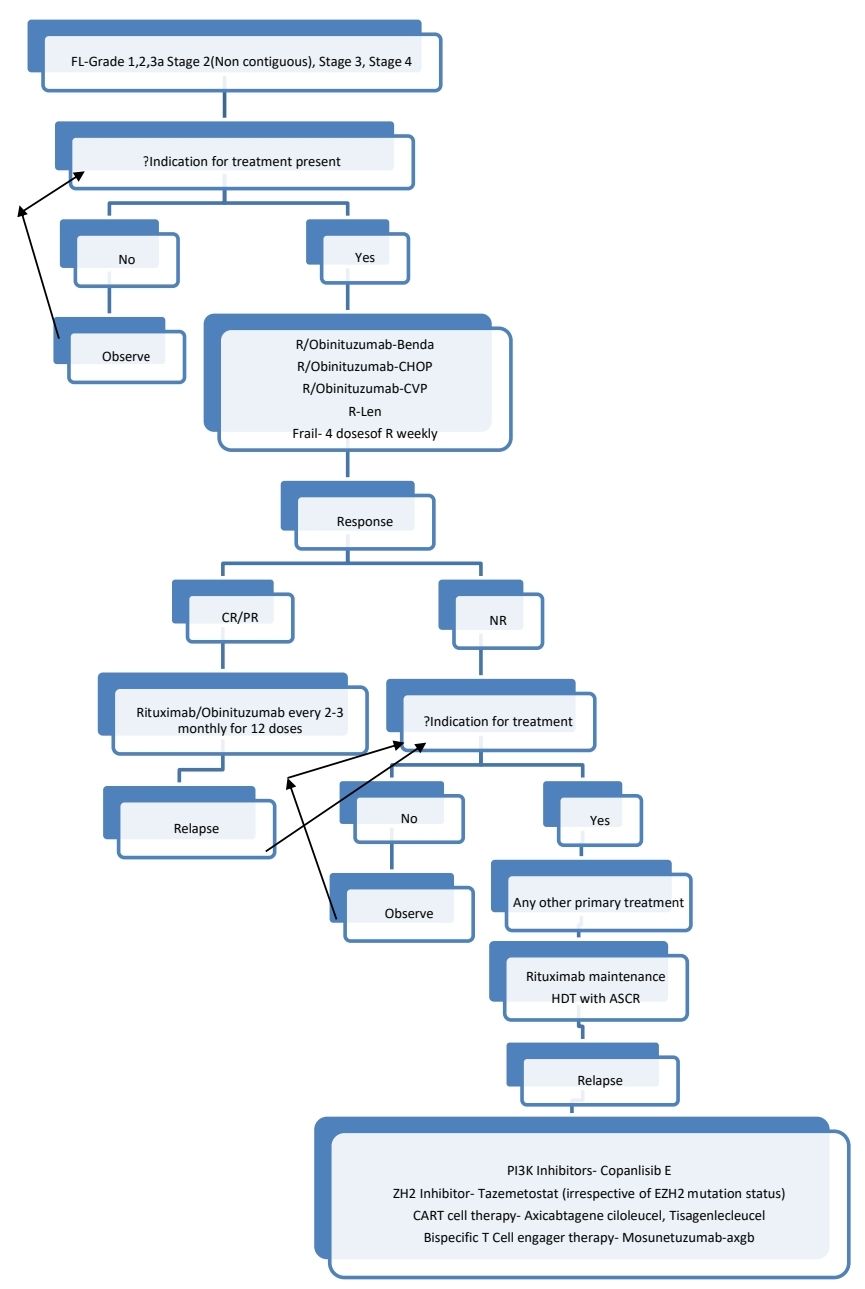
Follicular lymphoma Grade 3 is treated according to DLBCL protocol
Follicular lymphoma with transformation must be treated like DLBCL/ Double hit lymphoma. For all these patients do HDT with ASCR.
Relapsed follicular lymphoma:
- Treatment is necessary only if there is any one of indication for treatment.
- Choice of therapy depends on fitness of patient and previous treatments. Use alternate therapies, than those used previously. If there was long remission with primary therapy, same therapy can be readministered.
- Fit patients must be offered consolidation with high dose therapy with autologous stem cell therapy. If there is relapse after HDT with ASCR, allogeneic stem cell transplantation with RIC conditioning should be considered.
- For patients who are not fit for HDT with ASCR, maintenance with Rituximab (12 doses) must be given.
- Other options of therapy include
- Idelalisib- 100mg- BD. Common side effects include diarrhea, fatigue, rash and respiratory complications.
- Radio-immunotherapy- Y-90-Ibritumomab tiuxetan and I-131- Tositumomab
- Short course low dose radiotherapy
- Single agent Rituximab- For frail patients
- Drugs under trial- Lenalidomide, Duvelisib, CAR-T cell therapy
About Each Modality of Treatment:
- ISRT- 24 Gy in 12 fractions (curative intent), 4 Gy in 2 fractions (Palliative intent)
- Chemotherapy: Choice is based on factors such as age, comorbidities, future treatment possibilities (Ex:HDT wih ASCR)
Supportive Care:
- All patients must receive prophylaxis with Aciclovir and cotrimoxazole
Follow up of patients who are not on treatment:
- Once in 3-6 months- History, physical examination and labs to determine the rate of disease progression. Repeat imaging is done only if clinically indicated. LDH level should not be performed routinely.
Monitoring After Treatment/ Follow-up:
- History, examination and labs 3-6 monthly for 5 years and then annually/ as clinically indicated
- CT (C/A/P)- every 6 monthly for 2 years and after that once a year
Special Situations:
- Transformation to high grade lymphoma
- 20-30% show transformation to high grade lymphoma.
- Annual rate of transformation- 3-4%
- Consider this possibility when
- LDH is rising
- Single site growing disproportionately
- Development of extranodal disease
- PET- Marked FDG avidity
- Biopsy should be done from most FDG avid area
- Poor prognosis with median survival of 6-20 months
- Treatment is similar to DLBCL/Double hit lymphoma
- HDT with ASCR is advised to patients who were previously treated for follicular lymphoma/transformed follicular lymphoma. HDT with ASCR is not necessary for those who have never received systemic therapy.
- Giving maintenance Rituximab does not improve overall outcome. Hence, it is not routinely recommended.
Related Disorders:
- Follicular lymphoma with 1p36 deletion
- Predominantly involve inguinal nodes and form large localized masses
- Predominantly diffuse pattern in histopathology, typically grade 1-2
- CD23 positive
- Good prognosis
- Should be treated as stage 1 or Stage 2 (Contiguous)- Non-bulky follicular lymphoma
- Large B cell lymphoma with IRF4/MUM1 rearrangement
- They are usually follicular lymphoma- Grade 3B
- Patients typically present with involvement of Waldeyer's ring
- Seen in children or young adults
- Locally aggressive disease
- Responds to chemotherapy +/- radiotherapy
- They must be treated like DLBCL
- Paediatric type follicular lymphoma
- Seen in young patients
- Male are commonly affected
- Presents as localized disease, especially in head and neck
- Lacks BCL2 expression or t(14:18)
- Express BCL6, CD10, +/-IRF4/MUM1 in 20% cases
- Treatment-
- Stage 1 and 2- Excision
- Stage 3 and 4- Chemotherapy (RCHOP)
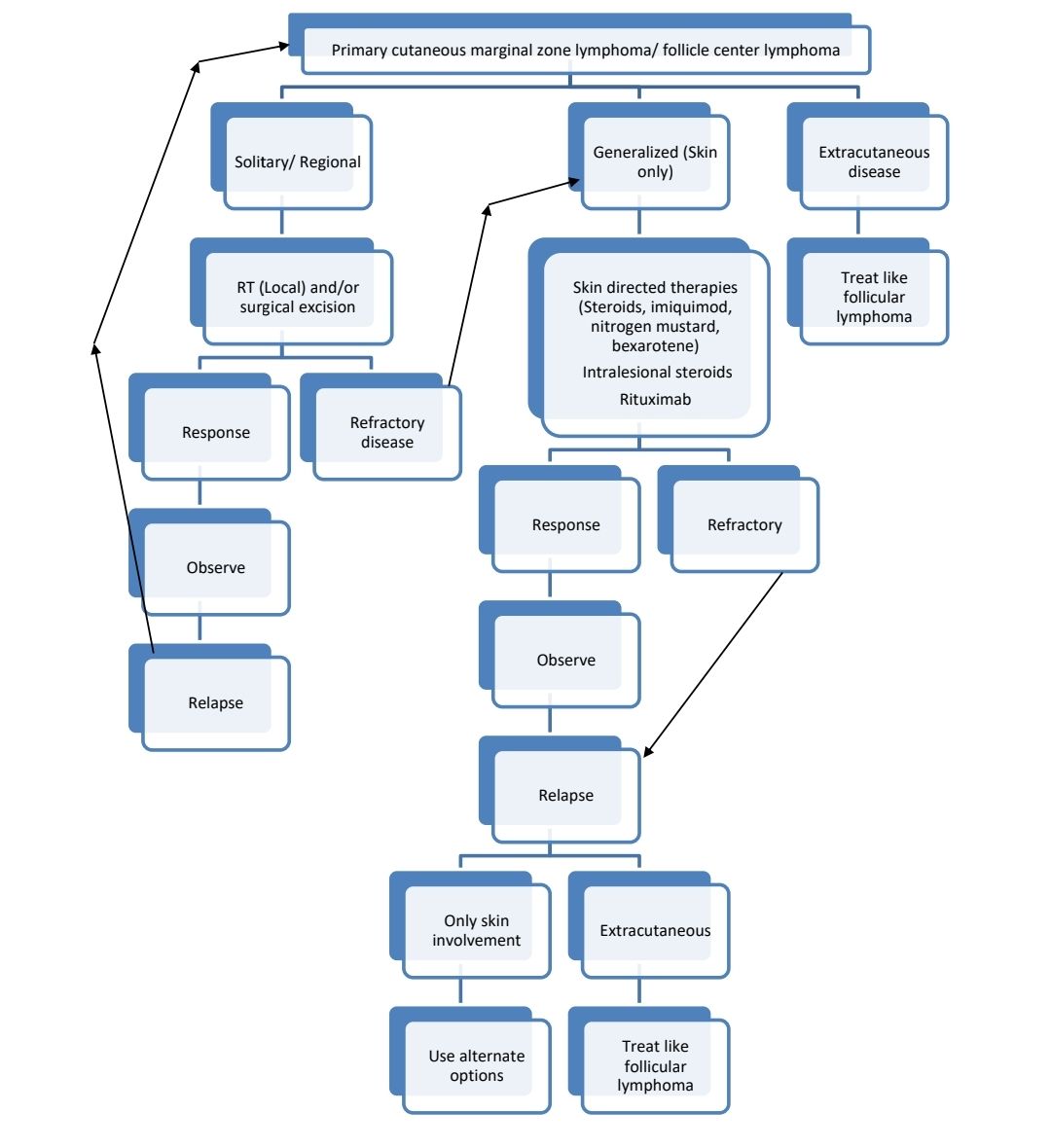
- Primary cutaneous follicle centre lymphoma
- Also called reticulohistiocytoma of dorsum or Crosti's disease
- Centrocytes and variable number of centroblasts with follicular, follicular+diffuse or diffuse growth pattern
- Presents as solitary skin nodule over head/trunk with surrounding erythema
- Indolent course. 5 year survival >95%
- Rarely disseminates
- BCL6- Positive, BCL2 negative
- Treatment plan:
- Duodenal type follicular lymphoma
- Majority occur in 2nd part of duodenum
- Excellent survival even without treatment
- Presents as small polyp, incidentally detected at endoscopy
- Wait and watch
- In symptomatic patients, treatment options include
- Radiotherapy
- Rituximab monotherapy
- Rituximab with chemotherapy
- Clarithromycin
- Intrafollicular/ in situ follicular lymphoma
- Morphologically normal lymph node morphology
- IHC shows some follicles which are BCL2 positive
- Also positive for CD10.
- Also positive for t(14;18)(q32;q21)/ IGH::BCL2
- Diagnosis of lymphoma should not be made in such cases
- Asymptomatic
- No treatment required- Wait and watch
- With 12 years follow up risk of transformation to overt FL is 5-10%
Recent advances:
Obinutuzumab with lenalidomide (GALEN Regimen) as upfront therapy in advanced follicular lymphoma (Results of LYSA study)
Induction treatment was obinutuzumab (1000 mg IV, days 8, 15, and 22, cycle 1; day 1, cycles 2-6) plus lenalidomide (20 mg/d, days 1-21, cycle 1; days 2-22, cycles 2-6) for six 28-day cycles. Maintenance included obinutuzumab (1000 mg every 2 cycles) plus lenalidomide (10 mg, days 2-22) for ≤12 cycles (year 1) followed by obinutuzumab (1000 mg every 56 days) for 6 cycles (year 2). The overall response rate in present study was 92%. Neutropenia was most common side effect which was mild in most of the patients. This study shows promising clinical efficacy with chemotherapy free GALEN regimen.
https://doi.org/10.1182/blood.2021013526
Response Adapted post-induction therapy in follicular lymphoma: Results of FOLL-12 study
This study involved total of 807 patients. Patients who ere PET and MRD negative were only observed. PET negative and MRD Positive patients were given 4 doses of weekly Rituximab, untill MRD was negative. PET and MRD positive patients were given Ibritumomab, followed by standard maintenance rituximab. Comparator arm received routine 2 years maintenance of Rituximab. Maintence therapy was found to superior, including in patients who were PET and MRD negative.
https://doi.org/10.1200/JCO.21.01234
Relevance of bone marrow biopsies for response assessment in follicular lymphoma
Bone marrow biopsies are performed before/after therapy to confirm complete response in patients with lymphoma on clinical trials. Present study sought to establish whether BMB add value in assessing response or predict progression-free survival or overall survival outcomes in follicular lymphoma subjects. Only 5/580 (0.9%) had positive baseline BMB, CR on imaging, and subsequent positive BMB. Therefore, BMB were irrelevant to response in 99% of subjects. Study recommended eliminating BMB from clinical trial requirements.
https://doi.org/10.1200/JCO.21.02301
Minimal residual disease status predicts outcome in patients with previously untreated follicular lymphoma
The study aimed to analyze minimal residual/detectable disease (MRD) as a predictor of outcome in previously untreated patients with follicular lymphoma (FL) from the GALLIUM trial. Patients received induction with obinutuzumab (G) or rituximab (R) plus various chemotherapy regimens, followed by maintenance with the same antibody in responders. MRD status was assessed at predefined time points. MRD positivity was associated with inferior progression-free survival (PFS) at multiple time points. Obinutuzumab-based chemotherapy resulted in higher MRD response rates compared to rituximab-based chemotherapy.
https://doi.org/10.1200/JCO.23.0083
Epcoritamab monotherapy in patients with relapsed or refractory follicular lymphoma
In the EPCORE NHL-1 phase 1–2 trial, the novel CD3 × CD20 bispecific antibody epcoritamab demonstrated significant efficacy in patients with multiply relapsed or refractory follicular lymphoma. In the pivotal cohort, the overall response rate was 82%, with a complete response rate of 62.5%. The cycle 1 optimisation cohort showed a reduced incidence of cytokine release syndrome to 49%, with no cases of severe neurotoxicity. Epcoritamab exhibited strong clinical activity and a manageable safety profile, highlighting its potential as a treatment option for this challenging patient population.
https://doi.org/10.1016/S2352-3026(24)00166-2
Acalabrutinib alone or in combination with rituximab for follicular lymphoma: An open-label study
In this open-label, parallel-group study, patients with relapsed/refractory (R/R) follicular lymphoma (FL) were randomised to either acalabrutinib monotherapy or acalabrutinib plus rituximab. An additional cohort of patients with treatment-naive (TN) FL received only the acalabrutinib-rituximab combination. Acalabrutinib-rituximab was well tolerated and active in R/R and TN FL; in the TN cohort the overall response rate was 92.3% with most remissions lasting over 4 years. Acalabrutinib monotherapy was also well tolerated and active in R/R FL. These results support further study of acalabrutinib alone and in combination with rituximab in FL.
https://doi.org/10.1111/bjh.19787
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.