howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Hemostasis
Structure of platelets:
- Platelets are disc shaped structures with smooth surface.
- They have several openings on the surface resembling holes in the sponge.
- Peripheral zone consists of
- Outer fluffy surface coat- Contains glycocalyx (glycoproteins, proteins and mucopolysaccharides)
- Phospholipid bilayer- Consists of phosphatidyl serine
- Integral proteins- such as GlycoproteinIb (receptor for vWF), IIa, IIIa (Receptor for fibrinogen), IX
- Structural zone (which consists of supporting structure)
- Microtubules- Consist of tubulin dimmers, which maintain the discoid shape
- Cytoskeletal network- Consist of actin, and various actin binding proteins
- Cytoplasmic meshwork- Consisting of actin and myosin
- Organellar zone (Responsible for storage and secretion of various substances)
- Granules
- Dense bodies- Consist of ATP, ADP, other nucleotides, serotonin and calcium
- Alpha granules- Consist of various hemostatic proteins such as fibrinogen, factor V, vWF, plasminogen activator inhibitor, alpha 2 antiplasmin,
- Lysozymes- Consist of enzymes
- Mitochondria- 4-5 mitochondria are present per platelet
- Glycogen- It is broken down to glucose 1 phosphate
- Granules
- Membrane system- Consist of
- Surface connected open canalicular system
- Dense tubular system which originates from rough ER
- Fused system- It connects above two systems.
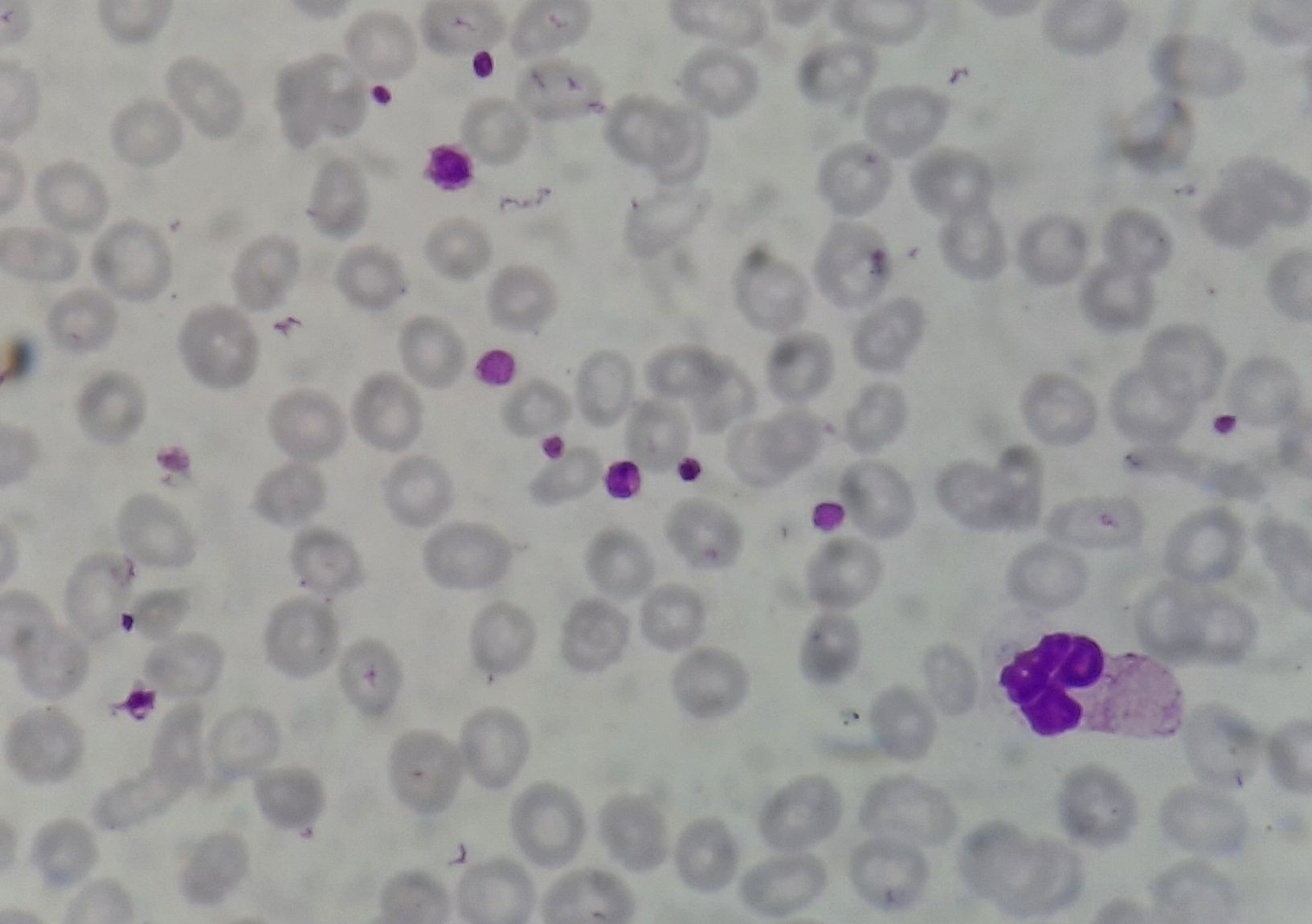
Figure 1.6.1 - Platelets in peripheral smear
3 phases of hemostasis:
- Vascular: Mediated by the release of locally vasoactive agents that result in vasoconstriction at the site of injury and reduced blood flow.
- Platelet: Aggregation of platelets to form platelet plug
- Plasma: Includes initiation, propagation and stabilization of clot.
Function of platelets:
- Wherever there is endothelial injury, platelets attach to exposed subendothelial collagen, which occurs with the help of von Willebrand factor (vWF connects Glycoprotein Ib/IIb on platelet surface to collagen)
- Upon binding of vWF with Glycoprotein Ib/IIb, enzymes (phospholipase C, A2 and adenyl cyclase) in the membrane of platelets are activated.
- Activated enzymes cleave specific membrane phospholipids, leading to release of specific 2nd messengers such as ionositoltriphosphate. Phospholipase hydrolyses arachadonic acid to form prostaglandins. Cyclooxygenase acts on arachadonic acid to form thromboxane A2.
- ADP and serotonin released from activated platelets induce recruitment of additional platelets.
- Inositoltriphosphate stimulates release of calcium from dense tubular system.
- Calcium causes changes in proteins in structural zones, because of which there is change in shape of platelets, with formation of numerous pseudopods. Platelets can fit together in a “jig-saw puzzle effect”.
- There are 2 phases in aggregation of platelets
- Primary- Loose adherence
- Secondary- Firm adherence after release of ADP.
- Following adhesion of platelets, there is initiation of coagulation system by these mechanisms
- Attachment of fibrinogen to glycoprotein IIb/IIIa
- Change in membrane surface of platelets (exposing negatively charged phospholipids) which allows coagulation factors to bind to it.
- Activated platelets recruit blood borne tissue factor
- They also synthesize tissue factor
- Formation of procoagulantmicrovesicles
- Exposure of activated Factor V which is present within the platelets
- Thrombin generated during coagulation mechanism further activates platelets.
Coagulation pathway
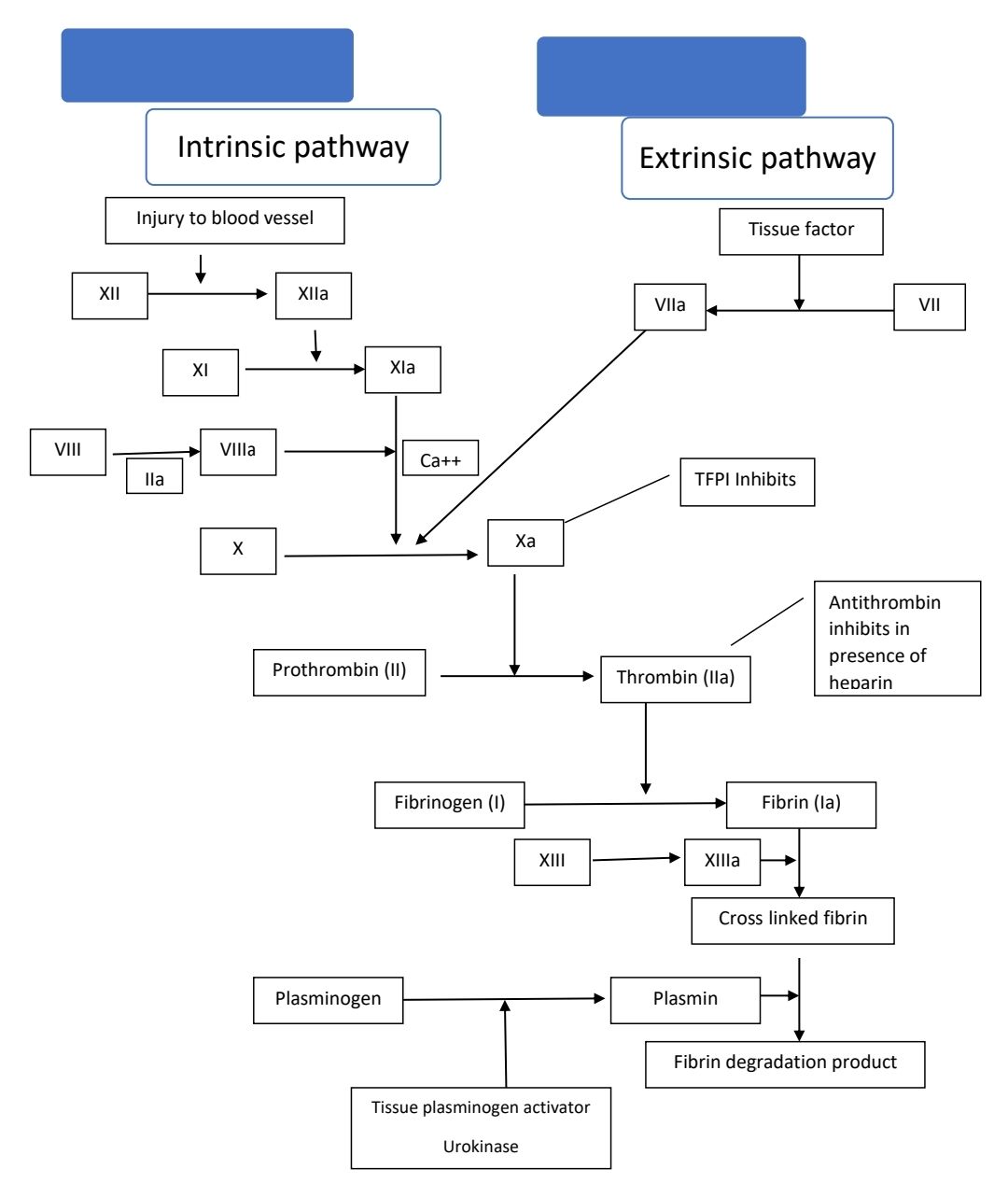
Figure - Coagulation and fibrinolytic pathway
- Classification of factors needed in coagulation pathway
- Zymogens
- Structurally all are similar and their gene structures are also similar. But they have highly specific functions, due to surface loops that are not homologous.
- All are synthesized in liver
- All are precursors of serine proteases that must be proteolytically activated to express their enzymatic activity.
- They are classified into 2 types
- Vitamin K dependent factors (Need gamma carboxylation at amino terminal of glutamic acid)- They include Factors 2, 7, 9, 10, and protein C
- Non Vitamin K dependent- They include factors 11, 12, prekallikrien, 13, thrombin activable fibrinolysis inhibitor
- Cofactors
- Soluble- factor 5, 8, vWF, protein S, protein Z, high molecular weight kininogen
- Cellular- tissue factor, thrombomodulin
- Structural proteins- Fibrinogen
- Inhibitors- Antithrombin, tissue factor pathway inhibitor, protein Z dependent protease inhibitor
- Zymogens
- Blood coagulation occurs when the enzyme thrombin is generated and proteolyses soluble, plasma fibrinogen, forming the insoluble fibrin polymer or clot.
- Initiation phase:
- Tissue factor is both necessary and sufficient to initiate coagulation in vivo.
- Tissue factor- VIIa complex (extrinsic tenase complex) activates Factor X to form Xa.
- Xa along with Factor Va, which is released from platelets, forms prothrombinase.
- Prothrombinase converts prothrombin to thrombin.
- Thrombin amplifies the coagulation loop by cleaving factor VIII from vWF, activating Factor VIII and Factor XI. This results in further release Factor V.
- Production of small amount of thrombin is sufficient to initiate events, that “prime” the clotting system for subsequent burst of thrombin generation.
- Propagation phase:
- Factor IXa (which is formed by action of Factor XIa or TF-FVIIa complex on Factor IX) binds to Factor VIIIa to form potent intrinsic tenase complex.
- Large amount of Factor X is converted to Factor Xa, ultimately leading to formation of large amount of thrombin.
- Large amount of thrombin, converts fibrinogen to fibrin, resulting in clot formation
- Stabilization phase
- Thrombin also activates Factor XIII, which cross links the fibrin and forms a stable clot.
- Thrombin activable fibrinolysis inhibitor also helps in this process. It removes lysine residues from the fibrin clot, thereby limiting plasmin binding.
Feedback inhibition of coagulation
- Excess of thrombin at the margin of clot binds to thrombomodulin (a receptor expressed on the surface of intact endothelium). Upon this binding thrombin acquires anticoagulant property and converts protein C to activated protein C.
- Activated Protein C, together with Protein S inactivate Factors Va and VIIIa
- Tissue factor pathway inhibitor, a protein produced from endothelium, inhibits VIIa/TF complex and Factor Xa.
- Antithrombin released at the margins of endothelial injury binds to thrombin and inactivates it. Antithrombin also inactivates Factor Xa.
Fibrinolysis
- Starts once the vessel injury is healed.
- Tissue plasminogen activator is activated when it binds to the lysine residues of fibrin. TPA activity is inhibited by plasminogen activator inhibitor 1.
- Tissue plasminogen activator and urokinase convert plasminogen to plasmin.
- Annexin A2 also augments formation of plasmin
- Plasmin causes degradation of fibrin via interaction with lysine and argenine residues.
Functions of fibrin degradation products
- Inhibition of platelet function
- Potentiation of hypotensive effects of bradykinin
- Chemotaxis
- Immune modulation
Role of endothelium in coagulation
- Antithrombotic properties
- Antiplatelet: Intactness, Production of nitric oxide and prostaglandins, synthesis of adenosine diphosphatase
- Anticoagulant- Membrane associated heparin like molecules activate antithrombin 3, production of thrombomodulin and tissue factor pathway inhibitor
- Fibrinolytic- Production of tissue type plasminogen activator
- Prothrombotic
- Platelets- Production of vWF
- Procoagulant- Production of tissue factor
- Antifibrinolytic- Production of inhibitors of plasminogen activator
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.