howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Pancytopenia
Updated on 28.03.2025
Introduction:
- It is a condition in which there is decrease in all three blood cell lines: RBCs, WBCs, and platelets.
Causes:
- Drugs:
- NSAIDs:Aspirin, Diclofenac, Ibuprofen, Indomethacin, Phenylbutazone, Salicylates, Sulindac, naproxen, piroxicam,
- Anti-gout: Allopurinol, Colchicine
- Antimicrobials: Albendazole, Chloramphenicol, Cidofovir, Dapsone, Foscarnet, Ganciclovir, Linezolid, Quinidine, Quinine, Sulfonamides, Zidovudine, streptomycin, chloroquine,
- Anti-epileptics: Carbamazepine, Fosphenytoin, Felbamate, Levetiracetam, Phenytoin, Phenobarbital, Valproate
- Anti-thyroid: Methimazole, Propylthiouracil, carbimazole,
- Cardiovascular: Amiodarone, Captopril, Lisinopril, Nifedipine, Quinidine, Ticlopidine
- Diuretics: Acetazolamide, Furosemide, Thiazides
- Psychiatric: Bupropion,Carbamazepine, Lithium, Valproate
- Chemotherapeutic agents: Alkylating agents, antimetabolites
- Others: Azathioprine, Cimetidine,Mesalamine, Sulfasalazine, Leflunomide, Methotrexate, Penicillamine, Benzene, MDMA (ecstasy), Glue vapors, Pesticides (lindane, organochlorine and organophosphate pesticides), organic arsenicals, gold
- Hypersplenism
- Nutritional deficiencies:
- Megaloblastic anemia: Vitamin B12 deficiency/ Folate deficiency
- Copper deficiency
- Alcoholism
- Anorexia nervosa/ prolonged starvation
- Vitamin D deficiency
- Immunological problems:
- Systemic lupus erythematosus (medications, infections, splenomegaly, autoimmune fibrosis, HLH, autoimmune destruction of cells)
- Sjogren syndrome
- Rheumatoid arthritis/ Feltry syndrome (Disease related or due to development of LGL leukemia)
- Eosinophilic fasciitis
- Sarcoidosis
- Autoimmune lymphoproliferative syndrome
- Common variable immunodeficiency
- Thymoma/ thymic carcinoma
- Pregnancy
- Infections:
- Viral infection: Covid-19, Hepatitis (Non ABCDEG), CMV, HIV, EBV, Parvo virus B-19, measles, influenza, hhv6 etc
- Overwhelming infection/sepsis
- Mycobacterial infection
- Brucellosis
- Ehrlichiosis
- Leishmaniasis
- Disseminated fungal infection
- Inherited disorders: (Marrow aplasia is seen in childhood and are associated with multiple organ involvement)
- Fanconi anemia
- Dyskeratosis congenita
- Shwachman-Diamond syndrome
- Reticular dysgenesis
- Pearson syndrome
- Familial aplastic anemia (autosomal and X-linked forms)
- Non-hematological syndromes (Down syndrome, Dubowitz syndromes, Noonan syndrome, cartilage hair hypoplasia)
- Other rare syndrome- Ataxia-pancytopenia (Myelocerebellar disorder), DNA ligase IV deficiency, Nijmegen breakage syndrome, reticular dysgenesis, Seckle syndrome
- Telomeropathies: Deficient telomerase repair/ inadequate telomere protection (Shelterin proteins)
- Telomeres are small repetitive hexamer DNA sequences located at the edge of chromosomes. They protect chromosomes from genetic material being lost after each cell division.
- DKC1, TERT, TERC, RTEL1 mutations lead to early telomere shortening
- Disturbed Hayflick phenomenon (Apoptosis after certain level of telomere shortening)
- Associated with early hair graying, pulmonary fibrosis and hepatic cirrhosis
- Poor response to immunosuppressive therapy and bone marrow transplant, but good response to high dose androgens
- Higher risk of MDS and AML
- Others:
- Transfusion associated GVHD
- Orthotopic liver transplantation with fulminant hepatitis
- Aplastic crisis in hemolytic anemias
- Whole body irradiation-Doses >1.5-2 gray to whole body (In this condition supporting marrow matrix is damaged, so BMT is unsuccessful)
- Osteopetrosis
- Hyperparathyroidism
- Storage disease: Goucher disease, Niemann-Pick disease etc
- Metastatic solid tumors
- Hematological malignancy:
- Hypocellular: Hypoplastic myelodysplastic syndrome, Hypoplastic AML, Hypocellular ALL/ Partially treated ALL, Hairy cell leukemia, Lymphoma- HD/NHL (as some of the tumor cells induce bone marrow hypoplasia)
- Hypercellular: AML, ALL, Lymphoma, Hairy cell leukemia, myeloma, LGL Leukemia, MDS
- Other haematological disorders:
- Myelofibrosis: Primary and secondary
- Paroxysmal nocturnal hemoglobinuria
- Hemophagocytic lymphohistiocytosis
- Idiopathic aplastic anemia
- Idiopathic cytopenia of undetermined significance (Cytopenia which remains undiagnosed for more than 6 months despite of adequate evaluation)
Investigations:
- CBC
- Peripheral smear: Look for
- Macrocytic RBCs, macro-ovalocytes and hypersegmented neutrophils in megaloblastic anemia
- Virocytes in EBV, dengue or other viral infection associated pancytopenia
- Schistocytes in case of sepsis related DIC
- Blasts/ abnormal promyelocytes
- Hairy cells or atypical lymphoid cells of NHL spill over
- Pseudo Pelger Huet anomaly and cytoplasmic hypogranularity in MDS
- Leukoerythroblastic reaction with tear drop cells in myelofibrosis
- Vitamin B12 levels and LDH
- LFT
- Ferritin, S. Triglycerrides and fibrinogen levels
- USG abdomen: To note splenomegaly, metastasis in liver etc
- Bone marrow aspiration and biopsy- with
- Flow cytometry
- Cytogenetics
- PNH work up
- NGS for MDS related mutations EX: SF3B1, TET2, SRSF2, DNMT3A, ASXL1
- S. Ferritin, Triglyceride- for HLH
- Skull X ray lateral view and protein electrophoresis- For myeloma
- HIV, HBsAg, HCV, Parvo, EBV, CMV, HSV, VZV
- SBDS gene study
- ANA profile
- S. Calcium and PTH levels
- Blood culture
- Fanconi testing
- Telomere length analysis
Note:
- Nearly 50% of pancytopenia in India are secondary to megaloblastic anemia. Hence if there is macrocytosis, increased LDH/ decreased vitamin B12 levels, avoid further evaluation such as bone marrow aspiration and biopsy.
- In some selected cases consider therapeutic trial of Vitamin B12
- Some of the pancytopenia are multifactorial. Examples include:
- Alcohol, megaloblastic anemia, hypersplenism
- HIV infection, HAART therapy and AIDS associated lymphoma
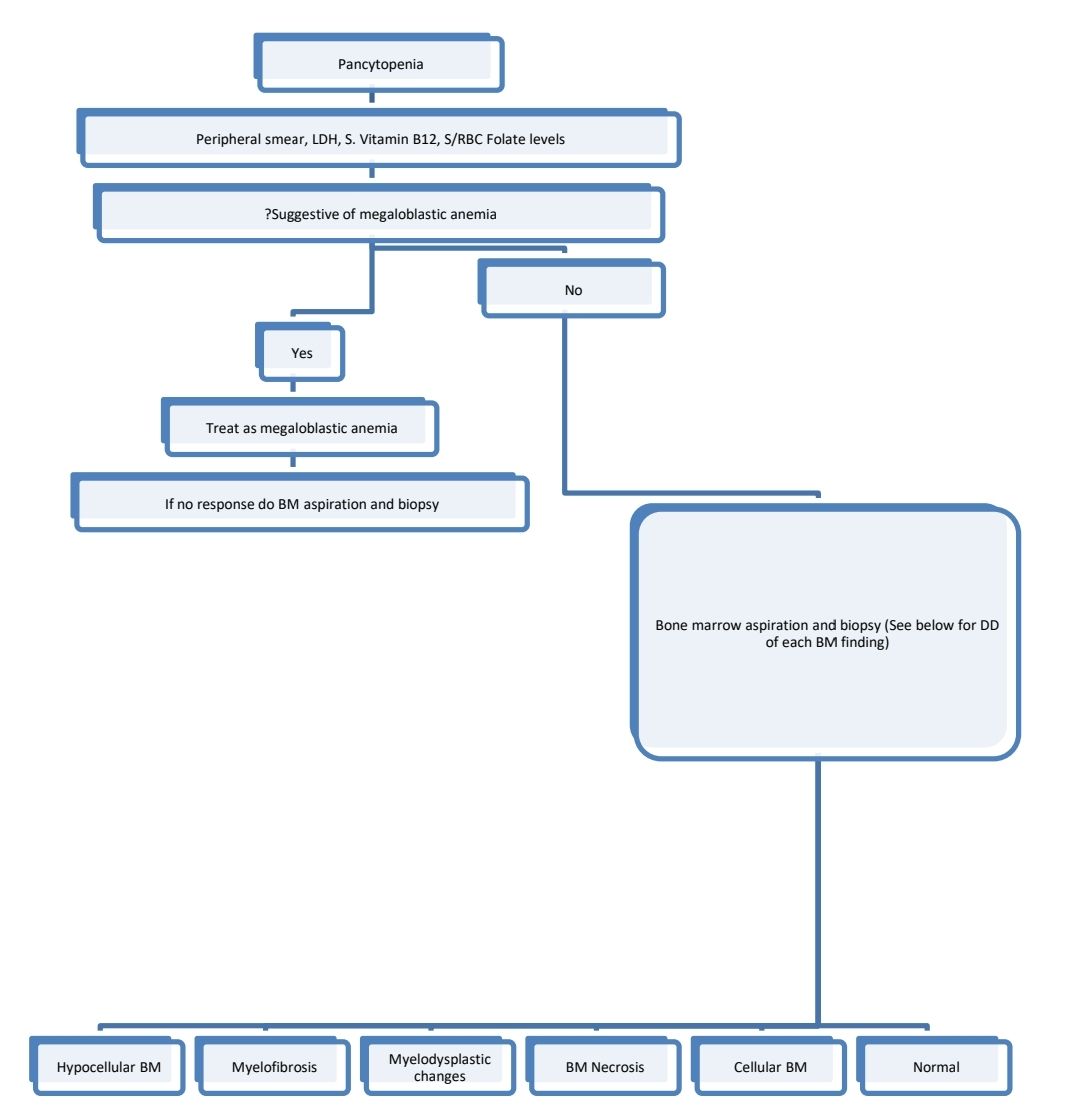
Diagnostic algorithm
- Hypocellular BM
- Hypocellular MDS/ AML/ ALL
- Partially treated ALL
- Hairy cell leukemia
- T-LGL/ NHL/ Hodgkin's lymphoma
- Drug/ Chemical/ Radiation induced BM aplasia
- Virus associated aplastic anemia (Hepatitis, HIV etc)
- Autoimmune disease associated aplastic anemia
- PNH
- Anorexia nervosa
- Vitamin B12 and folic acid deficiency
- Vitamin D deficiency
- Mycobacterial infection
- Aplastic crisis in haemolytic anemia
- Transfusion associated GVHD/ Liver transplant related aplastic anemia
- Inherited bone marrow failure syndromes (These may not have typical congenital anomalies at diagnosis. Hence stress cytogenetics/ NGS Panel for aplastic anemia is must before finalizing the diagnosis as Idiopathic acquired aplastic anemia in patients aged less than 40 years. This differentiation is essential as otherwise patient may be subjected to unnecessary transplant/ ATG therapy, transplant regimens may prove to be very toxic or donor may also have mutations related to IBMFS)
- If all above diseases are ruled out- Idiopathic aplastic anemia
- Myelofibrosis
- Infections:
- HIV
- Disseminated tuberculosis
- Histoplasmosis
- Visceral Leishmaniasis
- Some viral infections such as EBV
- Autoimmune disorders:
- SLE
- Sjogren’s syndrome
- APLA syndrome
- Juvenile idiopathic arthritis
- Primary autoimmune myelofibrosis
- Scleroderma
- Chronic inflammatory condition
- Toxic chronic myelopathy
- Hematological disorders:
- Hairy cell leukemia
- MDS with fibrosis
- Mastocytosis
- HL/ NHL / Multiple myeloma/ Acute leukemia/ CML/ CMML/ Eosinophilic leukemia/ PNH/ Other MPN in fibrotic phase
- Acute panmyelosis with myelofibrosis
- TAFRO (thrombocytopenia, anasarca, fever, reticulin fibrosis and organomegaly)
- Metastatic carcinoma (Esp breast, prostate etc)
- Treatment with growth factors:
- Recombinant human thrombopoietin agonists, for example, romiplostim
- IL-11, Ex: oprelvekin
- Osseous and other metabolic diseases:
- Renal osteodystrophy
- Vitamin D deficiency
- Hyperparathyroidism
- Osteopetrosis
- Paget’s disease
- Radiation exposure
- Grey platelet syndrome
- Benzene exposure
- If all above are ruled out- Primary myelofibrosis
- Infections:
- Myelodysplastic changes
- Megaloblastic anemia
- Heavy metal toxicity
- Alcohol abuse
- HIV, Parvovirus
- Antitubercular therapy
- Drugs- MMF, chemotherapy, valproate
- PNH
- Copper deficiency
- Chronic liver disease
- If all of the above are ruled out- Myelodysplastic syndrome
- BM Necrosis
- Tumors- ALL, MPN, HL, solid tumors
- Infections- Sepsis, TB
- Drugs- Chemotherapy, interferons
- Sickle cell disease
- DIC
- HUS
- APLA
- Hyperparathyroidism
- SLE
- Anorexia nervosa
- Radiation exposure
- Markedly thickened bony trabeculae:
- Osteopetrosis
- Paget’s disease
- Vitamin D deficiency
- Hyperparathyroidism
- Hypophosphatasia
- Renal osteodystrophy
- Myelofibrosis in late stage
- Prior radiation therapy
- Metastatic disease
- Ghosal hematodiaphyseal dysplasia
- Mutations within the thromboxane synthase gene TBXAS1
- Cellular BM
- Malignancy- Acute leukemia, lymphoma, myeloma, metastasis
- HLH
- Osteopetrosis
- Megaloblastic anemia
- Goucher disease/ Niemann Pick disease
- Tuberculosis
- Sarcoidosis
- Normal BM or Hypercellular marrow without specific pathology
- Autoimmune cytopenia
- PNH
- Alcohol induced BM suppression
- Sepsis related cytopenia
- Drug/ radiation induced cytopenia
- Viral infection related cytopenia
- Hypersplenism related pancytopenia
Idiopathic cytopenia of undetermined significance (ICUS)
- It is single or multiple blood cytopenias that remain unexplained despite an appropriate evaluation (including bone marrow examination) and do not have a known associated clonal genetic alteration.
Unexplained cytopenia:
- It is a case of cytopenia in which cause of cytopenia could not be detected with conventional tests and cytopenia cannot be attributed to concomitant diseases
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.