howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Polycythemia
Updated on: 22.04.2025
Introduction
- It is condition where hematocrit/ hemoglobin are above upper limit of normal. (Hct- >0.52 in men, >0.48 in women or Hemoglobin >16.5gm/dL in men and >16gm/dL in women)
- RBC count is not used for defining polycythemia, as patients with thalassemia trait have high RBC count, but are anemic.
- 2.5% of normal population can have hemoglobin of >16.5gm/dL, as normal values are calculated with 95% confidence limits.
- Normally rate of production is adjusted to maintain red cell mass of 30ml/kg.
- Production and presence of increased number of red cells is associated with effects generated by changes in blood viscosity and volume .
- At Hct>50%,viscosity increases logarithmically which leads to decreased blood flow and O2 transport.
- Morphology and volume of marrow is only moderately altered (except in cases of polycythemia vera), as mere doubling of red cell production increases red cell mass to 60ml/kg.(In hemolytic anemia, increase occurs to 4- 6 times)
Causes of polycythemia:
- Primary (Low EPO levels)
- Polycythemia Vera
- Hereditary polycythemia-
- Erythropoietin receptor mutation leading to augmented response to EPO.
- EGLN1- Encodes Proline hydroxylase 2
- EPAS1- Encodes HIF-2 alpha
- Secondary (Elevated EPO level)
- Hypoxia-
- Pulmonary disease: Ex: chronic obstructive lung disease
- Alveolar hypoventilation:
- Central form: Cerebral vascular accident, Parkinsonism, encephalitis
- Peripheral form: Myotonic dystrophy, spondylitis, severe obesity (Pickwickian syndrome)
- Sleep apnea
- Right to left shunt- Eisenmenger syndrome
- High altitude
- Smoking
- Carboxyhemoglobinemia- Smoking, Carbon monoxide poisoning
- Autonomous EPO production from tumors- HCC, RCC, cerebellarhemangioblastoma, pheochromocytoma, parathyroid adenoma, meningioma, dermoid cyst of ovary, parotid tumors, uterine leiomyoma, TEMPI Syndrome (Telangiectasias, Elevated EPO levels, Monoclonal gammopathy, Peripheral fluid collection, Intrapulmonary shunting)
- Drugs- Sunitinib, Sorafinib, VEGF receptor inhibitor, androgens, growth hormone, erythropoietin, anabolic steroids, antidiabetic agents such as SGLT2 inhibitors (eg, canagliflozin, empagliflozin, dapagliflozin, ertugliflozin)
- Cobalt- Increases the levels of hypoxia inducible factor 1
- Nickel
- Exogenous EPO administration (Doping)
- Renal polycythemia: Post renal transplant (?AT2 signaling), Solitary renal cyst, Polycystic kidney disease, hydronephrosis, renal artery stenosis
- High O2 affinity hemoglobin, 2,3 Bisphosphonate deficiency, congenital methemoglobinemia
- Endocrine abnormalities: Cushing syndrome, primary aldosteronism, acromegaly , pheochromocytoma
- Inherited polycythemia (Due to gain/ loss of function germline mutations)
- CYB5R3- Cytochrome B5 reductase (Associated with congenital methemoglobinemia)
- BPGM- Bisphosphoglyceromutase
- HBA1/2, HBB- Globin chain variants with high oxygen affinity
- Hypoxia-
- Mixed primary and secondary.
- Chuvash polycythemia- High EPO polycythemia due to mutation of von HippelLindau gene.
- Relative/spurious polycythemia/ Hemoconcentration (normal red cell volume with reduced plasma volume)
- Dehydration
- Diuretics
- Loss of fluids into third spaces
- Large amounts of alcohol
- Smoking
- Gaisbock syndrome (Polycythemia hypertonia)
- Hyper-transfusion.
- Approximately 2.5% of healthy individuals have a higher hematocrit, as normal reference ranges are based on values within ±2 standard deviations, excluding those outside this range.
Clinical manifestations
- Rubor- Due to excessive deoxygenation of blood following sluggish flow through dilated cutaneous vessels (Plethoric appearance).
- Due to increased viscosity and vascular dilation: Headache, dizziness, chest/abdominal pain, weakness, fatigue, blurred vision, slow mentation, tinnitus, paresthesia, feeling of fullness in face and head.
- Cyanosis- Due to >4g/dl deoxygenated hemoglobin or >1.5g/dl of methemoglobin
- Hemorrhage (Nasal/stomach)- Due to capillary distension and ischemia due to circulating stagnation
- Thrombosis
- Common with polycythemia vera and not with other polycythemias
- Can be arterial or venous
- Pruritus-often present in polycythemia vera
History:
- Hyperviscosity symptoms: Chest/ abdominal pain, myalgia, weakness, fatigue, headache, blurred vision, transient loss of vision, paresthesia, slow mentation etc
- Thrombosis: especially at unusual sites
- Symptoms associated with PV: Unexplained fever, sweats, weight loss, pruritus (especially after bathing), erythromelalgia (intense burning pain in extremities), gout, early satiety due to splenomegaly
- History suggestive of volume depletion: Diuretics, vomiting, diarrhea, anorexia, orthostatic symptoms, CNS problems
- Cardiopulmonary disease- Dyspnea, chronic cough, cyanosis, sleep apnea- snoring/ hypersomnolence, mucocutabeous telangiectasias (indicate pulmonary AV malformations)
- History related to intra-abdominal tumor: Unexpected weight loss, hematuria, abdominal/ pelvic pain
- History of renal transplantation
- Smoking
- Exposure to carbon monoxide at work place
- Athlete with h/o doping
- Use of anabolic steroids for increasing muscle mass
- Family h/o polycythemia
Examination:
- Signs of dehydration- thirst, loss of skin turgor, orthostatic hypotension, elevated blood urea nitrogen/creatinine
- Scratch marks- Indicate pruritus in case of polycythemia vera
- Nicotinic stains on nails/ teeth
- Body mass index- Helps in identifying obstructive sleep apnea
- Cyanosis in lips, earlobes and fingers
- Clubbing
- Plethoric facies
- Breathing pattern
- Organomegaly/ intra-abdominal masses
- Bruit- Heard in case of renal artery stenosis
Investigations:
- Hemogram: Neutrophilia and thrombocytosis are present in PV, slightly00 high TLC is seen in smokers
- Arterial O2 saturation: To identify tissue hypoxia
- Pulse oxymetry may be used. Should be performed at rest and after moderate exertion. It can be misleading in carbon monoxide poisoning, high affinity hemoglobin and sleep apnea syndromes. SpO2 of <92% is associated with absolute erythrocytosis.
- S. Erythropoietin levels
- It should be done in non-phlebotomized patient
- Low levels seen in PV and primary familial polycythemia
- Increased in secondary polycythemia
- Considerable overlap exists
- S. Uric acid: Increased in PV
- S. Ferritin level- Low in polycythemia vera
- S. Calcium level- Helpful in detecting parathyroid adenoma
- Chest X ray- To rule out lung problems such as COPD
- Bone marrow aspiration and biopsy:
- Not required for diagnosis of PV
- Increased trilineage hematopoiesis with eosinophilia and basophilia is seen in PV. Variation in megakaryocyte sizes including larger variants with uneven/ hypolobated nuclei are characteristically are seen in PV. Megakaryocyte clusters are commonly seen in PV.
- In others only erythroid hyperplasia is seen. There can be stromal inflammatory features like increased plasma cells, increased hemosiderin in stromal macrophages and evidence of abundant background apoptotic activity.
- Iron stores are reduced in PV.
- Helps in assessing degree of fibrosis. Increased fibrosis is noted in PV.
- Also provides baseline findings which can be compared with subsequent BM biopsies
- Karyotyping: Abnormalities are seen in 10-20% patients with PV. Commonly trisomy 8 and 9, del 20q, del 13q and del1p.
- MPN reflex panel on peripheral blood sample (by PCR/NGS) which includes
- JAK 2- V617F mutation- Seen in over 95% of PV patients. It can be sometimes positive in normal individuals also. Hence results must be interpreted with caution.
- JAK 2- exon 12 mutation
- mpl mutation
- Cal-R mutation
- USG abdomen and pelvis with renal doppler
- To know renal problems, hepatic pathology and uterine leiomyoma
- Splenic size also can be noted- Splenomegaly is seen in PV
- Doppler helps to identify renal artery stenosis
- Blood carboxy-hemoglobin levels
- Should be done in the evening after day's work of patient
- If levels are >5% of total hemoglobin, it indicates carbon monoxide poisoning.
- Sleep studies: to rule out sleep apnea syndrome
- Pulmonary function tests
- Hemoglobin disassociation curve- Left shifted curve indicates high affinity hemoglobin (P 50 is decreased).
- Hemoglobin electrophoresis: It can detect up to 50% of high affinity hemoglobins
- LFT and RFT- As number of renal and hepatic disorders can cause polycythemia
- Sleep study- Helps in identifying spleep apnea syndrome
- CT abdomen with pelvis-To know any tumors causing polycythemia.
- CT brain-If hemangioblastoma is suspected.
- Red cell mass determination
- It is done using isotopic dilution methodology, using patient's RBCs tagged with Technetium 99
- Helps in differentiating true from spurious polycythemia
- Expensive and often inaccurate
- Normal red cell mass is 24-30ml/kg
- Erythroid colony cultures
- To study their responsiveness to EPO
- Growth without adding EPO is seen in PV (Endogenous erythroid colonies)
- It is most specific test for PV
- It is expensive and laborious test
- Sequence analysis (NGS)
- EPO receptor gene and genes involved in oxygen sensing- VHL, EGLN1, EPAS1
- High affinity hemoglobinopathies- Mutations in globin genes- HBA1, HBA2, HBB, 2,3 biphosphoglycerate deficiency as a result of BPGM mutations
- Analysis of vHL, PHD2 and HIF2alfa genes
Compared to others in Polycythemia vera, there is usually splenomegaly, constitutional symptoms, aquagenic pruritus, erythromalalgia, venous thrombosis, leucocytosis, thrombocytosis, increased cobalamin levels, normal O2 saturation, low EPO levels, increased uric acid levels, pan-hyperplasia in bone marrow, decreased iron stores, cytogenetics abnormalities and positive mutation studies.
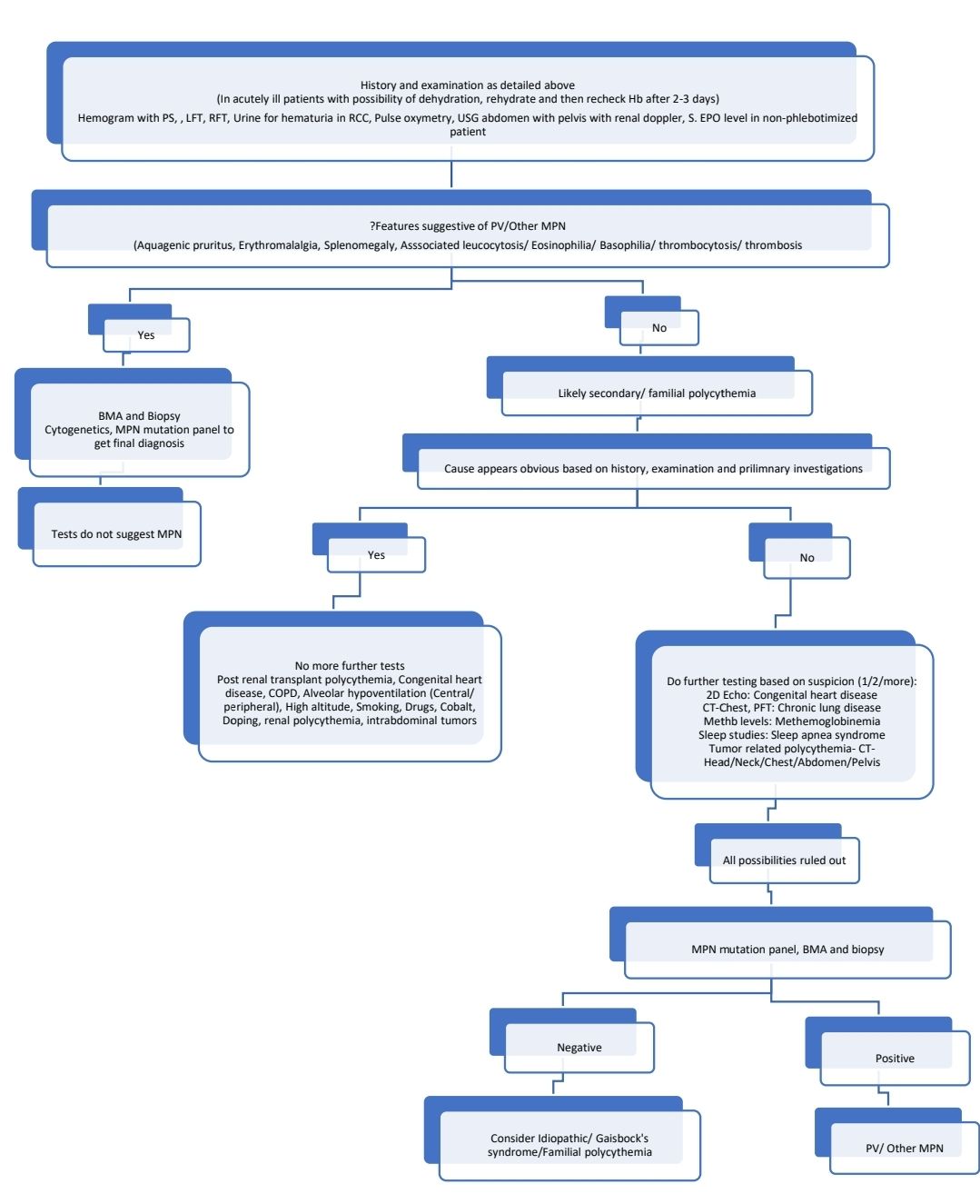
Diagnostic algorithm:
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.