howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Primary cutaneous T-cell lymphomas (Includes mycosis fungoides)
This category includes following disorders:
- Mycosis fungoides
- Subcutaneous panniculitis-like T-cell lymphoma
- Primary cutaneous CD30-positive T-cell lymphoproliferative disorders:
- Lymphomatoid papulosis
- Primary cutaneous anaplastic large cell lymphoma
- Primary cutaneous CD4-positive small or medium T-cell lymphoproliferative disorder
- Primary cutaneous acral CD8-positive T-cell lymphoproliferative disorder
- Primary cutaneous CD8-positive aggressive epidermotropic cytotoxic T-cell lymphoma
- Primary cutaneous gamma/delta T-cell lymphoma
Mycosis fungoides
Introduction:
- It is a malignant proliferation of mature memory T cells of helper type.
- Sezary syndrome is a generalized mature T cell lymphoma characterized by the presence of erythroderma, lymphadenopathy and neoplastic T-lymphocytes in the blood.
Epidemiology:
- Account for 50% of all cutaneous lymphomas
- M:F= 2:1
- Usually seen in adults
- Median age- 55 years
- Account for 1.5% of all lymphomas in US
Etiology:
- HTLV-1 in some cases
- Occupational exposure to petrochemicals
Pathogenesis:
- Prolonged antigenic stimulation leads to enhanced immune response, subsequently there are mutations affecting apoptotic pathway.
- Homing of tumor cells in skin by following mechanisms
- Cutaneous lymphocyte antigen binds to e-selectin of dermal venules
- CCR4 chemokine receptor on tumor cells binds to c-c chemikines ligands (17 and 22) in skin.
- CXC chemokine receptor 3 and 4- Binds to integrin receptors on dermal Langerhans cells
Clinical Features:
- Inflammatory premycotic phase
- Widespread, patchy, scaly, erythematosus pruritic eruptions
- Bathing trunk distribution- Folds and non-sun exposed body areas
- Plaque phase
- Well demarcated plaques especially over the trunk, measuring >5cm
- Associated with lymphadenopathy
- Tumor phase
- Skin tumors are formed which ulcerate and fungate
- Nonspecific scaly eruptions
- Dissemination erythroderma (Overlap with Sezary syndrome)
- Sezary syndrome: Erythroderma, Pruritus, Alopecia, Palmar or plantar hyperkeratosis, Onychodystrophy
- D’emblee lesions – skin tumors without preceding patch / plaque stage
- Lesions may lead to insomnia, weight loss, depression and suicidal ideations
- 50% deaths occur due to infections, usually due to staphylococcus/ pseudomonas. They start as cutaneous infections and then cause septicemia.
Investigations:
- Skin biopsy
- Epidermotropic infiltrates containing small to medium sized cells These cells contain irregular (cerebriform) nuclei.
- Poutrier microabscesses – Aggregates of cerebriform cells in the epidermis
- Epidermal involvement with single cell exocytosis.
- In the dermis, infiltrates may be patchy, band like or diffuse depending upon the stage of disease
- Inflammatory infiltrate consisting of small lymphocytes and eosinophils may be present.
- Large cell transformation: Large cells are present in >25% of lymphoid/ tumor cell infiltrates in skin lesion biopsy.
- Lymph node biopsy
- Category 1 (No involvement)- Dermatopathic lymphadenopathy, scattered cerebriform lymphocytes may be present, but clusters are not seen
- Category 2 (Early involvement)- Focal obliteration of architecture with clusters of atypical, cerebriform lymphocytes, often mainly paracortical in distribution.
- Category 3 (massive involvement)- Complete replacement of architecture with diffuse infiltrates of atypical, cerebriform lymphocytes
- Peripheral smear
- Neoplastic cells contain markedly convoluted nuclei. Cytoplasm is scanty, sometimes vacuolated
- Sometimes predominantly small (Lutzner cells) or large (Classical Sezary cell) are seen.
- Minimum of 1000 such cells / cmm must be present for diagnosis of Sezary syndrome
- Immunophenotyping
- Positive- CD2, CD3, CD5, CD4, TCRbeta, HECA antigen, Cutaneous lymphocyte antigen
- Negative – CD8, CD7, CD26, Cytotoxic associated proteins
- Molecular studies
- Clonal rearrangement of TCR genes
- Inactivation of CDK N2A/p16, PTEN
- Cytogenetics
- Complex karyotypes: usually involve chromosomes 6, 2, 1 and 17q
Criteria for Diagnosis:
Mycosis fungoides:
Essential:
- Presence of persistent and/or progressive patches and plaques especially in sun-protected areas (they may progress to form tumors in tumor stage)
- Presence of small to medium-sized atypical T cells with hyperchromatic hyperconvoluted (cerebriform) nuclei, preferentially in the epidermis
Desirable
- Loss of pan T-cell antigens
- Demonstration of clonal TCR gene rearrangements in skin biopsy in selected cases
Sezary syndrome:
Essential
- Erythroderma involving greater than 80% body surface area
- Evidence of blood involvement defined by demonstration of clonal TCR gene rearrangements
- Absolute Sézary cell count ≥1000/μL OR CD4/CD8 ratio >10 OR CD4+ CD7- cells ≥ 40% OR CD4+CD26- cells ≥30%
Staging of Mycosis fungoides :
Stage I | Disease confined to the skin Limited patches / plaques- <10% of BSA (stage Ia); disseminated patches / plaques (stage lb); skin Tumors (stage Ic). |
Stage II | Lymph nodes enlarged, but uninvolved histologically IIb- Skin tumors measuring >1cm. |
Stage III | Lymph node involvement documented by histology |
Stage IV | Visceral dissemination |
(Patient's palm without digits is equivalent to 0.5% of body surface area and with all 5 digits is equivalent to 1% of BSA)
Poor Prognostic Markers:
- Stage III or more
- Age > 60 years
- Increased LDH Levels
- Transformation to large T-cell lymphoma
- Presence of extracutaneous disease
- Peripheral blood involvement
Pretreatment Work-up:
- History
- Examination
- LN:
- Spleen:
- Skin-% BSA involved:
- WHO P. S.
- BSA
- IHC/Flow cytometry
- BMA and Bx
- Biopsy of suspected node
- CT (CAP)/ PET
- Stage
- Hemoglobin
- TLC, DLC
- Platelet count
- PS for Sezary Cells count
- LFT: Bili- T/D SGPT: SGOT: Albumin: Globulin:
- Creatinine
- Electrolytes: Na: K: Ca: Mg: PO4:
- Uric acid:
- LDH
- HIV:
- HBsAg:
- HCV:
- Serology for HTLV-1 (For high-risk population)
- UPT
- Chemotherapy consent after informing about disease, prognosis, cost of therapy, side effects, hygiene, food and contraception
- Fertility preservation
- PICC line insertion and Chest X ray after line insertion
- Tumor board meeting and decision
- Attach supportive care drug sheet
- Inform primary care physician
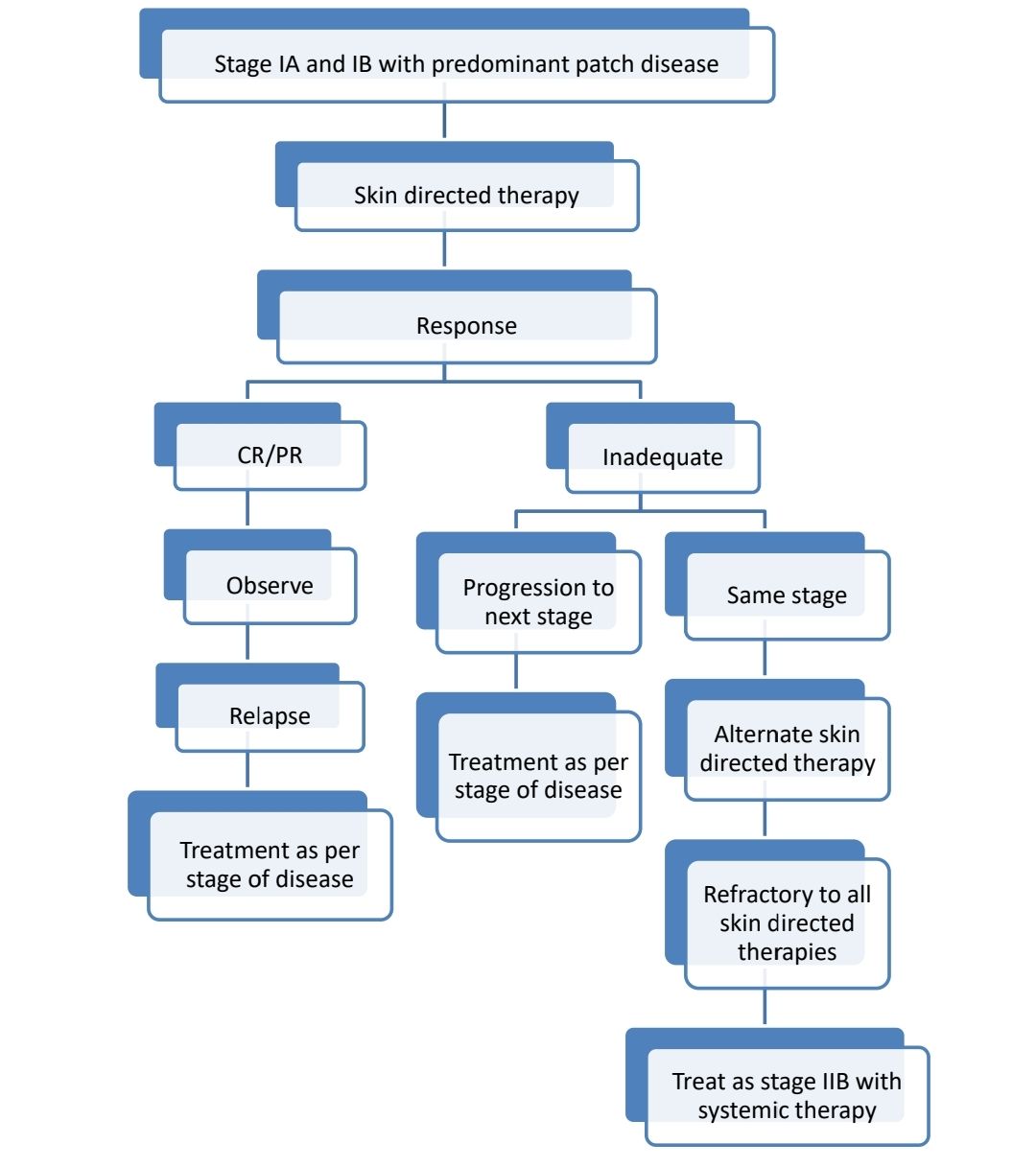
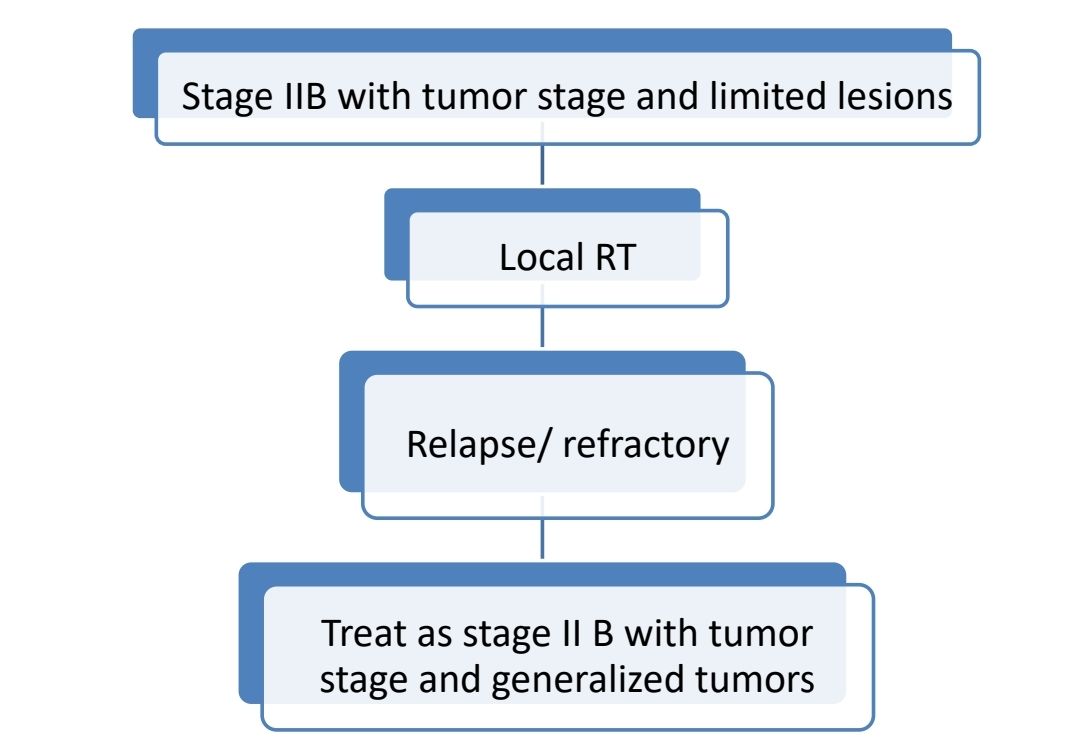
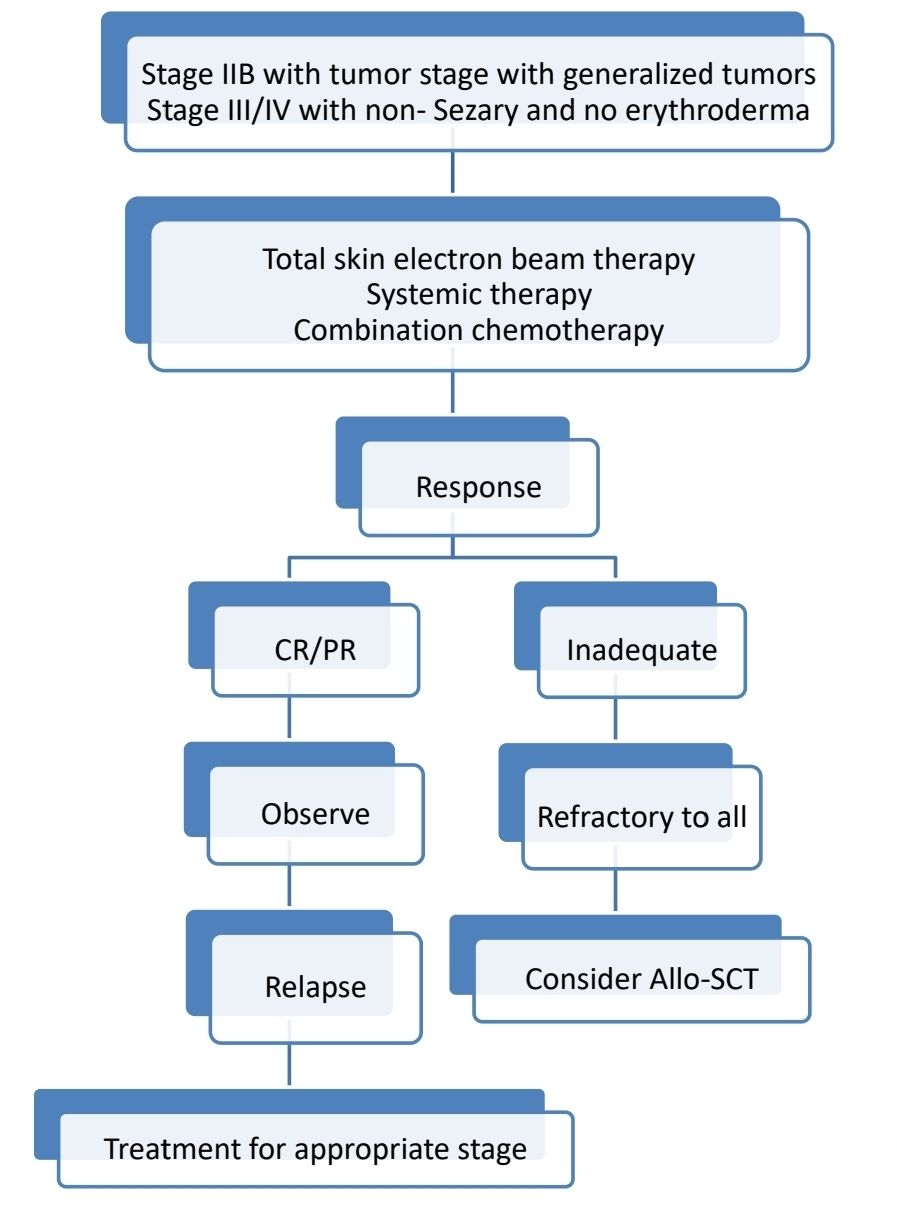
Treatment Plan:
Goals of therapy include:
- Reduce and control symptoms
- Minimise risk of progression
- Avoid treatment related toxicities. If chemotherapy is required, give single agents, rather than combination chemotherapies.
About Each Modality of Treatment:
- Skin directed therapies:
- Topical steroids
- Effective during early stages of MF
- Role is limited to temporary short-term use because of suppression of collagen synthesis (leading to skin atrophy), striae formation, skin fragility and secondary infections.
- Topical tacrolimus
- Advantage compared steroids is, it does not suppress collagen synthesis
- Topical imiquimod (Aldara)
- Topical immunomodulator
- Induces TNF alpha and INF
- Applied 3 times per week for 3 months
- Topical mechlorethamine
- Topical retinoids
- Bexarotene- 1% gel - LA- BD
- Binds to nuclear retinoid X receptors and alters gene expression
- Should not be given to pregnant ladies
- ISRT- 8-12 Gy
- Useful for localized plaques
- Phototherapy: UVB, PUVA/UVA1
- Given 3 times a week
- Minimum 4-8 weeks are required to achieve response
- Maintenance response is required after response (Once a week UVB)
- Electron beam therapy:
- Linear accelerator generated electron beams are scattered by penetrable plate placed at the collimeter site. Energy of electrons is reduced to 4-7 MeV which allows adequate field distribution
- Can be used for localized disease or entire skin surface.
- Remission rate- 80%
- 4Gy per week, to a total dose of 36 Gy in 8-9 weeks
- Advantages: Durable complete responses without systemic toxicity
- Disadvantages:
- Alopecia
- Atrophy, edema, dermatitis
- Increased risk of cutaneous malignancy
- Topical steroids
- Systemic therapy- Category 1
- Interferon alpha 2b
- Response rate: 50-70%
- Dose: 3-5x 106 Units/day or 3 times a week
- Side effects- Flu like symptoms, fatigue
- Methotrexate- <50mg/week
- Vorinostat
- Response rate: 30%
- Median time for recurrence- 56 days
- Side effects: Dairrhea, fatigue, nausea
- Brentuximab
- Bexarotine
- 300mg/m2 per day
- Response rate- 45-57%
- Side effects: Central hypothyroidism, pseudotumor cerebri, leucopenia, pruritus,
- Extracorporeal photopheresis
- 8-methoxy psoralen (0.6mg/kg) PO is given to patient
- White cells are collected, exposed to UVA and then reinfused
- It has direct cytotoxic effect on tumor cells and it also activates lymphocytes against tumor cells.
- Administered every 2-4 weekly until clearance of disease
- Response rate- 64%
- Interferon alpha 2b
- Systemic therapy- Category 2
- Gemcitabine
- Liposomal doxorubicin
- Pralatrexate
- Novel antifolate agent
- Dose: 15-30mg/m2- IV- Weekly- for 6-7 weeks
- Supplement folic acid
- Adverse effect- Mucosal inflammation, thrombocytopenia
- Systemic therapy for Relapse/ Refractory cases
- Chlorambucil
- Cyclophosphamide
- Etoposide
- Pentostatin
- Bortezomib
- Multiagent chemotherapy: Regimens similar to Peripheral T cell lymphoma (Results in increased immunosuppression with high risk of serious infections, resulting in death of patients in majority of patients)
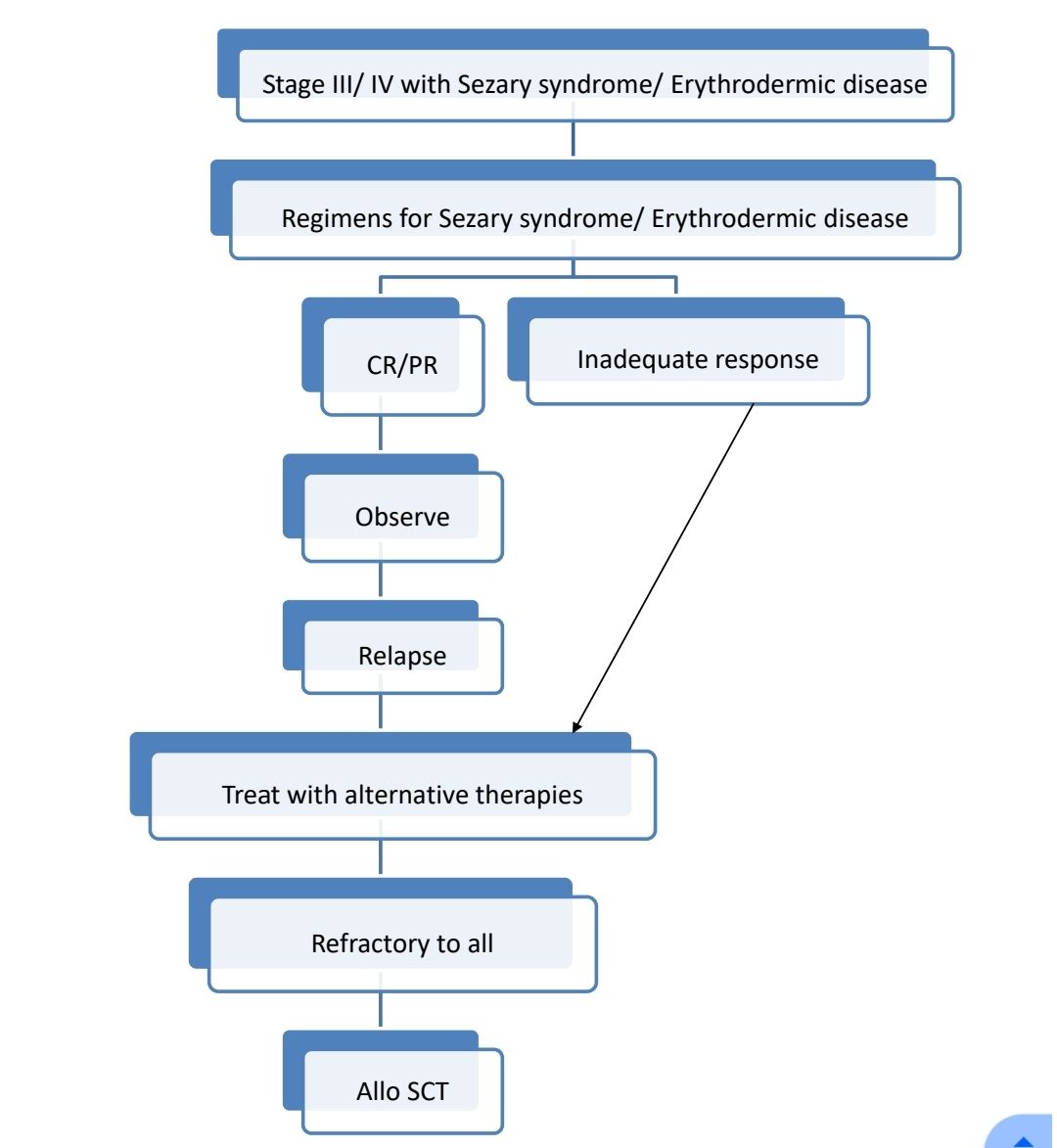
- Regimens for Eryhtrodermic lesions/ Sezary syndrome
- Phototherapy with Interferon alpha 2 b
- Phototherapy with retinoid
- Extracorporeal photopheresis with interferon/retinoid
- If high tumor burden (Absolute Sezary cell count- >5000/cmm)
- Same as above
- Mogamulizumab + Skin directed therapy
- Romidepsin + Skin directed therapy
Supportive Care:
- Pruritus
- Moisturizers, emollients and barrier protection
- Topical steroids with or without occlusion
- Optimize skin directed therapy
- Antihistaminics, Gabapentin
- Apprepitant, SSRI in selected patients
- Infections:
- Intranasal mupirocin
- Oral dicloxacillin
- Cotrimoxazole/ Doxycycline- if suspect MRSA
- Bleach baths or soaks
- Avoid central lines
Subcutaneous panniculitis-like T-cell lymphoma
Epidemiology:
- Very rare < 1% of all NHL
- Median age- 36 years
- 20% patients have associated autoimmune disease
Clinical Features:
- Multiple subcutaneous nodules (0.5cm-several cms)
- Extremities & trunk involved
- Rarely
- Hemophagocytic syndrome with pancytopenia
- Fever
- Hepatosplenomegaly
Investigations:
- Skin biopsy
- Infiltrate extends diffusely through the subcutaneous tissue
- Overlying dermis and epidermis and typically uninvolved
- Neoplastic cells are small with round nuclei and inconspicuous nucleoli and moderate amount of pale staining cytoplasm
- Rimming of the neoplastic cells surrounding individual fat cells
- Admixed reactive histiocytes are frequently present
- Marked tumor necrosis & karyorrhexis are common
- Vascular invasion may be seen
- Immunophenotyping
- Positive – CD8, CD2, CD3, Cytotoxic molecules (granzyme B, perforin, T cell intracellular Antigen)
- Negative: CD56, EBV markers
- Molecular studies-Rearrangements of TCR genes
Prognosis:
- Overall 5 year survival- 80%
- Poor Prognostic markers
- Dissemination to lymph nodes & other organs
- Hemophagocytic syndrome
Treatment:
- Initial disease control with steroids/ radiotherapy, then CHOP chemotherapy
Primary cutaneous CD30-positive T-cell lymphoproliferative disorders Lymphomatoid papulosis
Introduction:
- It is chronic recurrent skin disease characterized by the appearance of spontaneously regressing papules & an atypical T-cell infiltrate which can mimic a T-cell lymphoma histologically (strictly speaking it is not a lymphoma but may progress to lymphoma)
Clinical features:
- Skin papule / nodule, which regresses spontaneous within 3 – 6 weeks
Investigations:
- Biopsy of lesion:
- Wedge shaped dermal infiltrate consisting of T lymphocytes admixed with varying proportions of inflammatory cells such as neutrophils, eosinophils, macrophages & small lymphocytes
- Atypical T-lymphocytes resemble cerebriform cells
- Immunophenotyping: Atypical T cells – CD4+, CD8-, CD30 positive
Prognosis: Benign course
Treatment:
- Solitary/ Localized lesion: Radiotherapy alone
- Others:
- Low dose methotrexate (5-20 mg/week)
- Psoralen / UVA therapy
- Systemic retinoids
Primary cutaneous CD30-positive T-cell lymphoproliferative disorders: Primary cutaneous anaplastic large cell lymphoma
Epidemiology –
- 25% of T-cell lymphomas which arise in skin.
- Median age- 60 years
- M:F= 2-3:1
Clinical features
- Tumors / nodules / papules
- May show spontaneous partial / complete remission (but relapses are frequent)
Investigations
- Biopsy of lesion
- Similar to systemic anaplastic large cell lymphoma
- Pleomorphic, multinucleated giant cells and RS like cells are more numerous
- Infiltration is diffuse and involves both upper and lower dermis.
- Epidermal invasion and ulceration may be seen
- Immunophenotyping
- Positive – CD4, CD30, Cytotoxic granule associated proteins
- Negative – CD2, CD5, CD3, EMA, ALK protein
Prognosis:
- Good
- 5 year survival 90%
Treatment:
- Solitary lesions- Radiotherapy
- Others:
- Combination of PUVA and INF alpha
- Methotrexate (<100mg weekly)
- Systemic retinoids
- Pralatrexate
- Anti CD30 antibodies
- CHOP- Only in selected cases
Other cutaneous CD30-positive T-cell lymphoproliferative disorders:
- Systemic lymphoma Ex: ALCL, ATLL, PTCL, HL involving skin
- Other CD30 positive skin lymphomas: Transformed mycosis fungoides, cytotoxic T cell lymphoma
- Benign disorders: Lymphomatoid drug reactions, arthropod bites, viral infections
Primary cutaneous CD4-positive small or medium T-cell lymphoproliferative disorder
- Presents as solitary skin lesion, composed of CD4 positive pleomorphic T cells, without evidence of the plaques typical of mycosis fungoides
- Head and neck are commonly involved
- Benign clinical course, similar to cutaneous lymphoid hyperplasia
- Spontaneous regression after biopsy is seen in 1/3rd of patients
- Excellent prognosis with no risk of distant lymphoma in future
- Treatment:
- Intralesional steroids
- Surgical excision
- Radiotherapy
Primary cutaneous acral CD8-positive T-cell lymphoproliferative disorder
- Dermal, non-epidermotropic infiltrates of clonal medium-sized CD8+ cytotoxic lymphocytes
- Acral sites involved: Ears (MC), nose, hands and feet.
- Solitary, reddish, non-ulcerated papule or nodule
- IHC: CD3+, CD4-, CD8+, CD30- and betaF1+
- Complete remission after surgical excision/ local RT
Primary cutaneous CD8-positive aggressive epidermotropic cytotoxic T-cell lymphoma
- Neoplastic proliferation of T-lymphocytes often expressing CD8+ along with cytotoxic molecules
- Presents with papules, ulcerated nodules, tumours and plaques
- Micro: Dermal infiltration with pagetoid epithelial involvement, epidermal necrosis, high proliferative index
- Aggressive clinical behavior, mean survival- <12 months
Primary cutaneous gamma/delta T-cell lymphoma
- Clonal proliferation of mature, activated gamma delta T cells of Vδ1 or Vδ2 subsets
- Present as single or generalized skin and subcutaneous lesions
- IHC: TCR-gamma and TCR-delta positive and TCR-beta negative. CD3+, CD2+, CD7+/-, CD5-
- Aggressive course, median survival- <2 years
- Treatment: AlloSCT after initial high dose chemotherapy
Recent advances:
Ruxolitinib in HAVCR2 mutation-associated HLH and panniculitis
This study focused on six patients diagnosed with subcutaneous panniculitis-like T-cell lymphoma (SPTCL) associated with hemophagocyticlymphohistiocytosis (HLH) due to germline homozygous mutations of HAVCR2 (p.Y82C). The median age of onset was 10.5 years. Despite initial treatment with corticosteroids, immunosuppressants, or chemotherapy, responses were unfavorable. However, treatment with ruxolitinib, which targets inflammatory cytokines, resulted in rapid disease resolution and long-term remission.
https://doi.org/10.1111/bjh.18817
Allogeneic stem cell transplant for treatment of mycosis fungoides and Sezary syndrome
This meta-analysis assessed allo-HSCT outcomes for advanced-stage MF or SS based on 557 patients from 2010 to 2023. The results showed a 1-year overall survival (OS) of 51%, 3+year OS of 40%, and progression-free survival at 1 year and 3+ years of 42% and 33%, respectively. Non-relapse mortality was 18%, and relapse occurred in 47% of cases with a median time to relapse of 7.9 months. Rates of acute and chronic graft-versus-host disease were 45% and 40%. Reduced-intensity conditioning was associated with superior OS compared to myeloablative conditioning (58% vs. 30%). Donor lymphocyte infusion after relapse led to complete remission in 46% of cases.
https://doi.org/10.1038/s41409-023-02122-0
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.