howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Pure Red Cell Aplasia
Introduction:
- It is a condition in which there is isolated anemia which is secondary to failure of erythropoiesis.
- It is a syndrome characterized by
- Normocytic normochromic anemia
- Severe reticulocytopenia (absolute reticulocyte count- <10,000/cmm)
- Marked decrease/ absence of erythroid precursors in bone marrow (<3%) or maturation arrest at proerythroblast stage
Etiology
- Childhood PRCA
- Transient erythroblastopenia of childhood- Seen between 3 months and 4 years
- Transient aplastic crisis in hemolytic anemias (Parvo virus B-19 infection related)
- Fetal red cell aplasia: Non immune hydropsfetalis (In utero parvovirus-B-19 infection)
- Hereditary pure cell aplasia- Diamond Blackfan syndrome
- PRCA in adults
- Auto immune disorders – SLE, Rheumatoid arthritis, Sjogren syndrome, inflammatory bowel disease
- Tumors – CLL, large granular lymphocytic leukemia, lymphoma, thymoma, solid tumors (carcinomas of various organs)
- Drugs - Phenytoin, chloramphenicol, Azathioprine, INH, procainamide, sulphonamdies, allopurinol, ticlodipine, ribavarine, penicillamine, alemtuzumab, alpha nethyldopa, benzene, carbamazepine, chlorpropamide, cladiribine, cotrimoxizole, estrogen, fludrabine, gold, halothane, INF, lamivudine, linezolid, mycophenolate, penicillin, rifampicin, tacrolimus, zidovudine
- Pregnancy
- Infections- Parvo virus, Hepatitis virus, Adult T-cell leukemia virus, HIV, EBV, CMV, Mumps, Leishmaniasis, Grampositive systemic infections, Meningococcemia, Tuberculosis
- Others: Anti ABO antibodies in ABO incompatible BMT , Riboflavin deficiency, MDS (Primary myelodysplastic PRCA), Anti EPO antibodies (Prolonged EPO therapy in CKD patients)
- Primary
- Auto immune destruction of erythroid precursors which is mediated by
- T-lymphocyte induced direct cytotoxicity
- Ig G antibody (auto antibody) against erythroid precursor
- Cytokine mediated inhibition through FasL, IFN, TNF
- Direct toxicity by viruses
- STAT 3 gene mutation is seen in 40% of patients
- Auto immune destruction of erythroid precursors which is mediated by
Investigations:
- Peripheral smear
- Normocytic normochromic anemia
- White cells and platelets are normal
- Reticulocyte count – Markedly reduced
- Bone marrow examination
- Normal marrow cellularity
- Erythroid precursors are decreased- <5% proerythroblasts and basophilic erythroblasts is the criteria. But often <1% erythroids are seen.
- Normal myelopoiesis and megakaryopoiesis
- Flow cytometry- To rule out lymphoproliferative disorders such as CLL, NK-LGL, or T-LGL
- Parvovirus B19 testing by serology and PCR
- CT scan of chest- To rule out thymoma
- Cytogenetics- Abnormality indicates primary myelodysplastic PRCA
Pretreatment Work-up:
- History especially of offending drugs
- Examination
- WHO P. S.
- BSA
- BMA and Bx
- Cytogenetics
- Flow cytometry for CLPD panel
- Haemoglobin
- TLC, DLC
- Peripheral smear
- Reticulocyte count
- LFT: Bili- T/D SGPT: SGOT:
- Creatinine
- Electrolytes: Na: K: Ca: PO4:
- Uric acid
- LDH
- HIV:
- HBsAg:
- HCV:
- UPT
- ANA Profile:
- RA factor:
- Cytogenetics
- CT-Thorax
- USG- Abdomen
- ECHO- LVEF- %
- Parvo virus: IgG: IgM: PCR:
- CMV PCR:
- Tumor board meeting and decision
- Attach supportive care drug sheet
- Inform primary care physician
Treatment
- Secondary PRCA: Treatment of cause (See below)
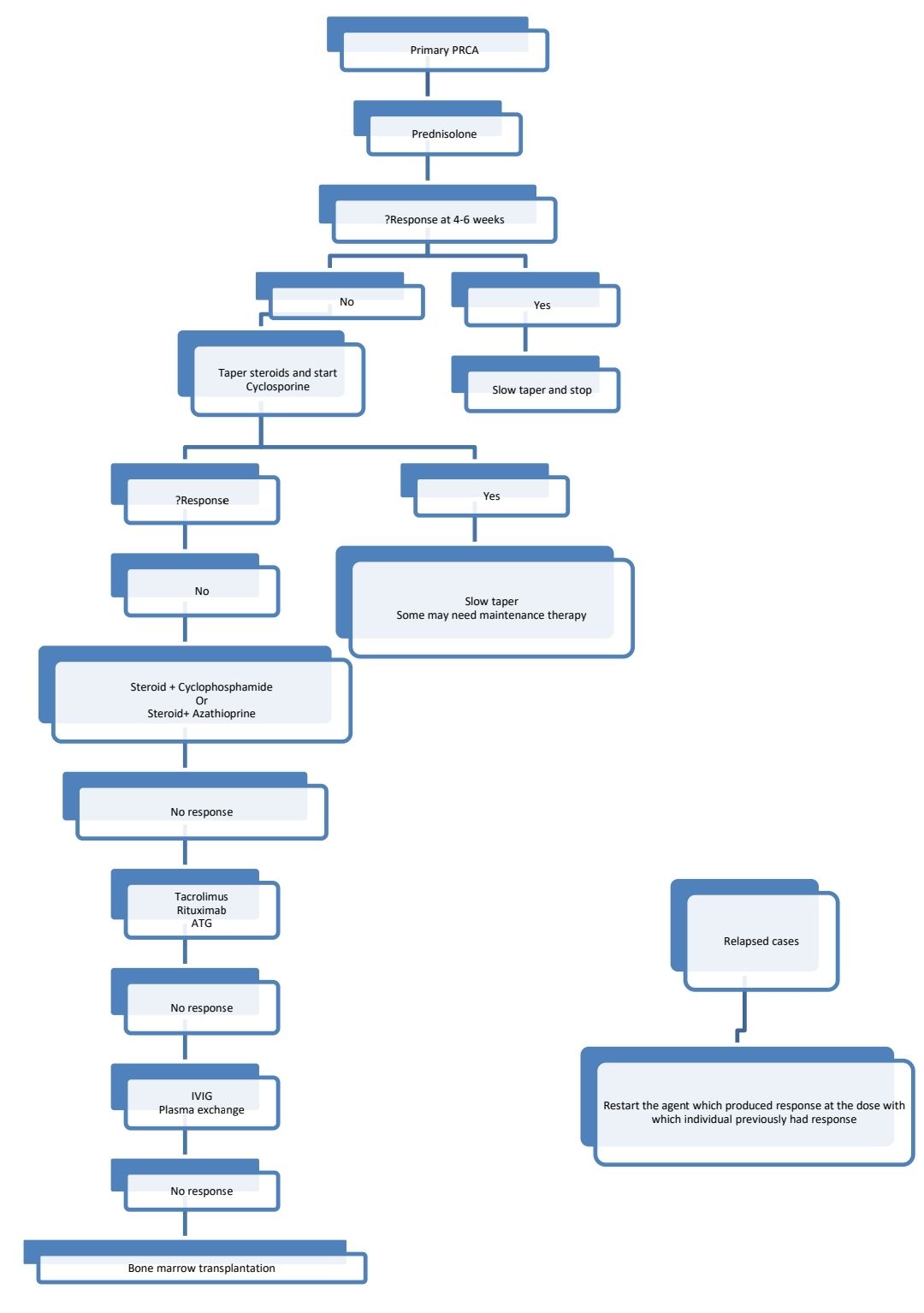
- Primary PRCA:
- Trial of vitamin B12 and folic acid
- Packed erythrocyte transfusions- To maintain hemoglobin between 7-9gm/dL
- Iron chelation based on ferritin
- Prednisolone
- Dose: 1mg/kg/day for 4 weeks
- Response rate- 40%
- Response is usually observed after 4-6 weeks
- Slow tapering is suggested over 3-4 months
- Ciclosporine
- More useful if LGL are seen in the peripheral smear.
- Maintain Trough levels between 200-300 microg/ml
- Cyclophosphamide- 50-150mg/day
- Azathioprine- 2-3mg/kg/day
- Immunosuppressive therapy with antithymocyte globulin and cyclosporine
- Rituximab- 375mg/m2 - weekly for 4 weeks
- Bone marrow transplant:PRCA is rarely an indication for SCT, as anemia can be managed with less drastic approaches. SCT is used in patients who fail all other medical line of treatment
- Other options:
- Methotrexate- 7.5-15mg per week
- Daclizumab (Anti IL2 antibody)-
- Effective in 40% of patients
- Dose- 1mg/kg- IV- every 2 weeks for at least 2 months
- Note: There is no use of androgens/ EPO/ Splenectomy
Subtypes of secondary PRCA
Parvovirus mediated PRCA
- Parvovirus B19 is a DNA virus that binds to P group antigen (globoside)
- It induces PRCA in immunocompromised patients and patients with increase cell turnover such as hemolytic anemia
- Presence of IgM antibody in absence of IgG antibody indicates acute infection
- PCR test is available and it is the test of choice
- Bone marrow shows giant pronormoblasts which contain markedly vacuolated, basophilic cytoplasm with pseudopodia and stippled chromatin and inclusion like nucleoli.
- Treatment
- Self limiting condition. Subsides once there is protective IgG response.
- Supportive transfusions
- IVIg is effective in AIDS patients (2gm/kg, divided over 5 days)
Anti-EPO antibody mediated PRCA
- Seen in cases who are on long-term use of EPO
- Risk factors
- Subcutaneous route of administration
- Use of EPO alfa stabilized in human serum albumin
- Use of silicone oil as lubricant in prefilled Eprex syringes
- Use in patients with chronic renal disease
- Antibody detection is possible by tests like ELISA
- Treatment
- Discontinuation of exogenous EPO including darbepoetin
- Immunosuppressive agents- Cyclosporine with or without steroids
- For patients with CKD- Plan renal transplantation
Thymoma related PRCA
- Treatment
- Resection of thymoma
- Thymectomy does not necessarily revert PRCA. Only 1/3rd experience remission.
- PRCA can follow thymectomy
Pregnancy related PRCA
- Most have resolution after pregnancy, hence give only supportive care
BMT associated PRCA
- Most of them have spontaneous resolution
- Treatment options include: Adjusting immunosuppression, DLI, plasma exchange, Rituximab
Myelodysplastic PRCA
- Treat as MDS
Diamond Blackfan Anemia
(Erythroblastopenia, Red cells agenesis, Aregenerative anemia, Congenital pure red cell aplasia)
Etiology:
- Inheritance- Autosomal dominant, Autosomal recessive
- Abnormality of gene in 1-Mb region on Chromosome 19q 13. (RPS-19 gene which encodes ribosome protein S 19)
- Another locus on Chromosome 8p 23.2-23.1
- Such many other genes have been identified such as RPS 19, 17, 24, RPL 35A and 11.
Pathogenesis
- Disease of ribosomal agenesis- Mechanism is not clear (First disease to be identified as ribosomopathy)
- There is defective maturation of r-RNA.Impaired ribosome function leads to impaired protein synthesis which causes early death of erythroid precursors by apoptosis
- Disorder of receptor ligand interaction between erythroid precursors and one/more growth factors is seen in some cases.
Clinical features:
- Considerable variation in phenotype is noted ranging from hydropsfetalis to presentation in adulthood
- Anemia
- Associated anomalies- Seen in 1/3rd patients
- Short stature and growth retardation
- Short webbed neck
- Sprengel deformity
- KlippelFeil deformity
- Face & head deformities – High arched palate, Cleft lip/ palate, hypertelorism, flat nasal bridge, microcephaly, micrognathia, microtia, low set ears, low hairline, epicanthus, snub nose, wide set eyes, thick upper lips, intelligent expression
- Hand deformities – Flat thenar eminence, triphalangeal thumb, syndactyly, bifid thumb, thumb duplication, thumb subluxation, thumb hypoplasia/ absence
- Genitourinary anomalies – Dysplastic/absent/horseshoe kidneys, hypospadias, renal tubular acidosis
- Cardiac anomalies – VSD, ASD, Coarctation of aorta
- Asplenia
- Opthalmic- Congenital glaucoma, strabismus, congenital cataract
- Learning difficulties/ mental retardation
Complications:
- Aplastic anemia
- MDS & AML
- Other cancers- Colon carcinoma, osteogenic sarcoma, female urogenital cancers etc
Differential Diagnosis
| DBA | Transient eythroblastopenia of childhood |
Pure red cell aplasia | Present | Present |
Age | Younger than 1 yr | Older than 1 yr |
Inheritance | Sporadic and dominant or possibly recessive inheritance, mutation analysis available for dBA1 (RPS19) | Not inherited |
Congenital anomalies | Present | Absent |
Mean corpuscular volume | Elevated | Normal |
Fetal hemoglobin | Elevated | Normal |
Red blood cell antigen | Present | Absent |
Erythrocyte adenosine deaminase activity | Elevated | Normal
|
Investigations:
- Peripheral smear- Macrocytic normochromic
- Reticulocyte count- Decreased
- Bone marrow aspiration: Normocellular marrow with marked erythroid hypoplasia
- Vitamin B-12 &folate levels – Normal
- Hb F – Increased to 5-25%
- I antigen on RBCs – Increased
- Serum iron &ferritin – Increased
- Transferrin Saturation – 100%
- Erythrocyte adenosine diaminase- Increased
- S. EPO- Increased
Diagnostic Criteria:
- Macrocytic normochromic anemia in first year of life
- Reticulocytopenia
- Normocellular marrow with marked erythroid hypoplasia
- Increased serum erythropoietin
- Normal or slightly decreased leukocyte count
- Normal or increased platelet count
- Rule out all other causes of PRCA such as transient erythroblastopenia of childhood, Pearson syndrome, Parvo virus B19 infection, HIV, drugs and toxins
Prognosis:
- If untreated, it is fatal.
- 40% children need long term packed cell transfusions
Treatment
- Corticosteroids
- Prednisolone- 2mg/kg/day in single dose in the morning
- Mechanism of action is not known
- 50%-70% patients respond
- Reticulocyte response is seen in 1-4 weeks, followed by rise in hemoglobin
- Once the maximum hemoglobin response (9-10gm/dL) is obtained prednisolone dose must be tapered slowly & patient is kept on lowest dose (If possible on an alternate day regimen)
- Many patients become steroid dependent
- Some centers start steroids after 1 year of age due to risk of growth failure.
- Predictors of response:
- Older age at presentation
- Family history
- Normal platelet count
- Blood transfusion to correct anemia.
- Correction must be moderate, as full correction suppresses erythropoiesis
- Maintain hemoglobin between 7-9gm/dL
- Do full RBC phenotype prior to first transfusion
- Use leucodepleted PCV to avoid allo-immunisation
- Chelation should be started early to prevent transfusionalhemosiderosis
- Splenectomy is indicated in the event of increased transfusion requirement
- For steroid resistant cases metoclopramide can be used.
- Stem cell transplantation- Curative treatment for steroid resistant cases.
Other treatment options (very poor response rates)
- IL 3
- High dose methylprednisolone
- Cyclosporine A
- Androgens
- Erythropoietin
- Leucine- Stimulates translation initiation factors that regulate binding of mRNA to ribosomal complex
Figures:
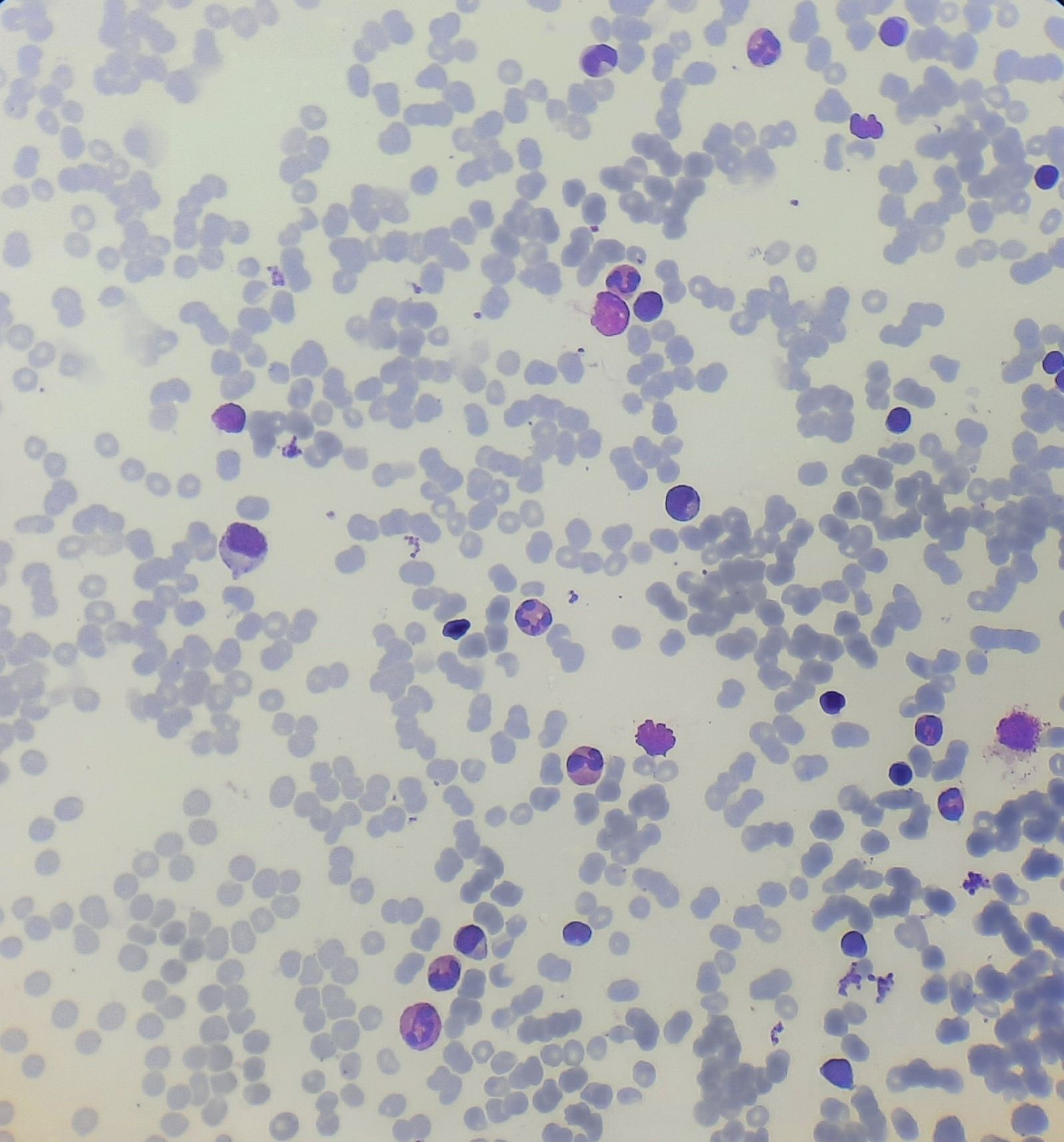
Figure 8.6.1- Pure red cell aplasia- Bone marrow aspiration
Recent advances:
STK10 mutations block erythropoiesis in acquired pure red cell aplasia via impairing ribosome biogenesis
In this study, whole exome sequencing of 30 newly diagnosed PRCA patients identified STK10 mutations as a potential driver. STK10 knockdown inhibited erythroid differentiation, reduced ribosome biogenesis, and activated the p53 pathway in K562 cells, leading to apoptosis and impaired erythropoiesis. These findings suggest that STK10 mutations contribute to acquired PRCA by disrupting ribosome production and activating pathological p53 signaling.
https://doi.org/10.1007/s00277-024-05802-z
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.