howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Splenomegaly
Introduction
- On ultrasonographic examination- if length of the spleen is more than 11cm, it is considered as splenomegaly
Causes:
- Congestive
- Right sided heart failure
- Budd Chiary syndrome
- Cirrhosis with portal hypertension
- Portal/ splenic vein thrombosis
- Non cirrhotic portal hypertension
- Hepatic schistosomiasis
- Infections
- Viral infections- HIV, Infectious mononucleosis, Dengue fever, Rubella, CMV, Herpes simplex, viral hepatitis
- Bacterial infections: Subacute bacterial endocarditis, brucellosis, tularemia, malidiosis, listeriosis, plague, secondary syphilis, relapsing fever, psittacosis, ehrlichiosis, tuberculosis, splenic abcess, typhoid, septicemia
- Rickettsial disease- Rocky mountain spotted fever, Q fever, typhus
- Fungal infections- Blastomycosis, histoplasmosis, systemic candidiasis
- Parasitic infections: Malaria, kala-azar, schistosomiasis, babenosis, coccidiodomycosis, paracoccidiodomycosis, trypanosomiasis, toxoplasmosis, ecchynococcosis, cysticercosis, visceral larva migrans
- Inflammatory/ Autoimmune
- SLE, Feltry syndrome
- Juvenile rheumatoid arthritis
- Autoimmune lymphoproliferative syndrome
- Hemophagocytic lymphohistiocytosis
- GVHD
- Serum sickness
- LGL leukemia
- Common variable immunodeficiency
- Anti D immunoglobulin administration
- Rheumatic fever
- Sarcoidosis
- Tropical splenomegaly
- Associated with hemolysis
- Thalassemia
- Pyruvate kinase deficiency
- Hereditary spherocytosis
- AIHA (rarely)
- Hemoglobinopathies- Sequestration crisis of sickle cell anemia, HbC and other hemoglobinopathies, certain variants of sickle cell anemia
- Infiltrative
- Nonmalignant: Splenic hematoma, Littoral cell angioma, lipid storage diseases (Goucher, Neimann Pick), Cystinosis, Amyloidosis, Multicentric Castleman disease, mastocytosis, Hyper eosinophilic syndrome
- Extrameduallry erythropoiesis- Myelofibrosis, osteopetrosis, thalassemia major
- Malignant
- Hematologic- CLL, CML, ALL, AML, PV, HCL, ET, Hepatosplenic lymphoma, HD, SMZL, NHL
- Non Hematological: Metastasis (rare), Neuroblastoma, Wilm's tumor, Leiomyosarcoma, Fibrosarcoma, Malignant fibrous histiocytoma, hemangiosarcoma, Kaposi's sarcoma, lymphangiosarcoma
- G-CSF/ EPO administration
(Causes of massive splenomegaly (enlargement beyond umbilicus) include- Myelofibrosis, CML, HCL, SMZL, CLL, Malaria, Leishmaniasis, Beta thalassemia major, Goucher disease, tropical splenomegaly, AIDS with MAC)
Investigations:
- Peripheral smear
- Pancytopenia- Seen in hypersplenism, lymphoma, HCL, Myelofibrosis, SLE
- Neutrophilic leucocytosis- Acute infections, inflammations
- Leucocytosis with premature white cells- CML, MF, MPN/MDS
- Blasts in acute leukemia
- Leucoerythroblastic blood picture- MF, BM infiltration
- Erythrocytosis- Polycythemia vera
- Atypical lymphocytes- Infectious mononucleosis and other viral infections
- Thrombocytosis- MPN, chronic infections like tuberculosis
- Parasites- Malaria, Bartonellosis, Babesiosis
- Hemolytic picture in hemolytic anemia
- Lymphocytosis- CLL, Lymphoma spill over
- Echocardiography- For heart failure, infective endocarditis
- Abdominal USG with portal venous doppler (splenoportal axis)
- LFT
- CXR and sputum AFB for tuberculosis
- HIV
- Monospot test
- Dengue- NS1, IgG and IgM
- Brucella
- Serology for Typhus
- HCV, HBsAg, Widal tests
- VDRL
- Rapid malaria test
- ANA, AntiDs DNA
- Ferritin, Triglyceride, LDH
- RA factor
- SPE for M band and abdominal fat pad- For amyloidosis
- Hemoglobin HPLC/ Electrophoresis
- DCT, ICT
- Blood culture
- PCR for psittacosis, Rickettsia, TB, CMV
- Bone marrow aspiration and biopsy- Flow cytometry and molecular studies for MPN if necessary
- If CT is done, do it with oral and IV contrast
- Oral contrast- Helps to delineate splenic tissue from stomach, small intestine and colon
- IV contrast: Better visualization of spleen
- Upper GI endoscopy- To rule out esophageal varices
- Stool for schistosoma eggs
- Splenic aspiration/ core needle biopsy: High false negative rates and has risk of splenic rupture
- Diagnostic splenectomy: It is done in cases where cause remains undiagnosed after extensive testing
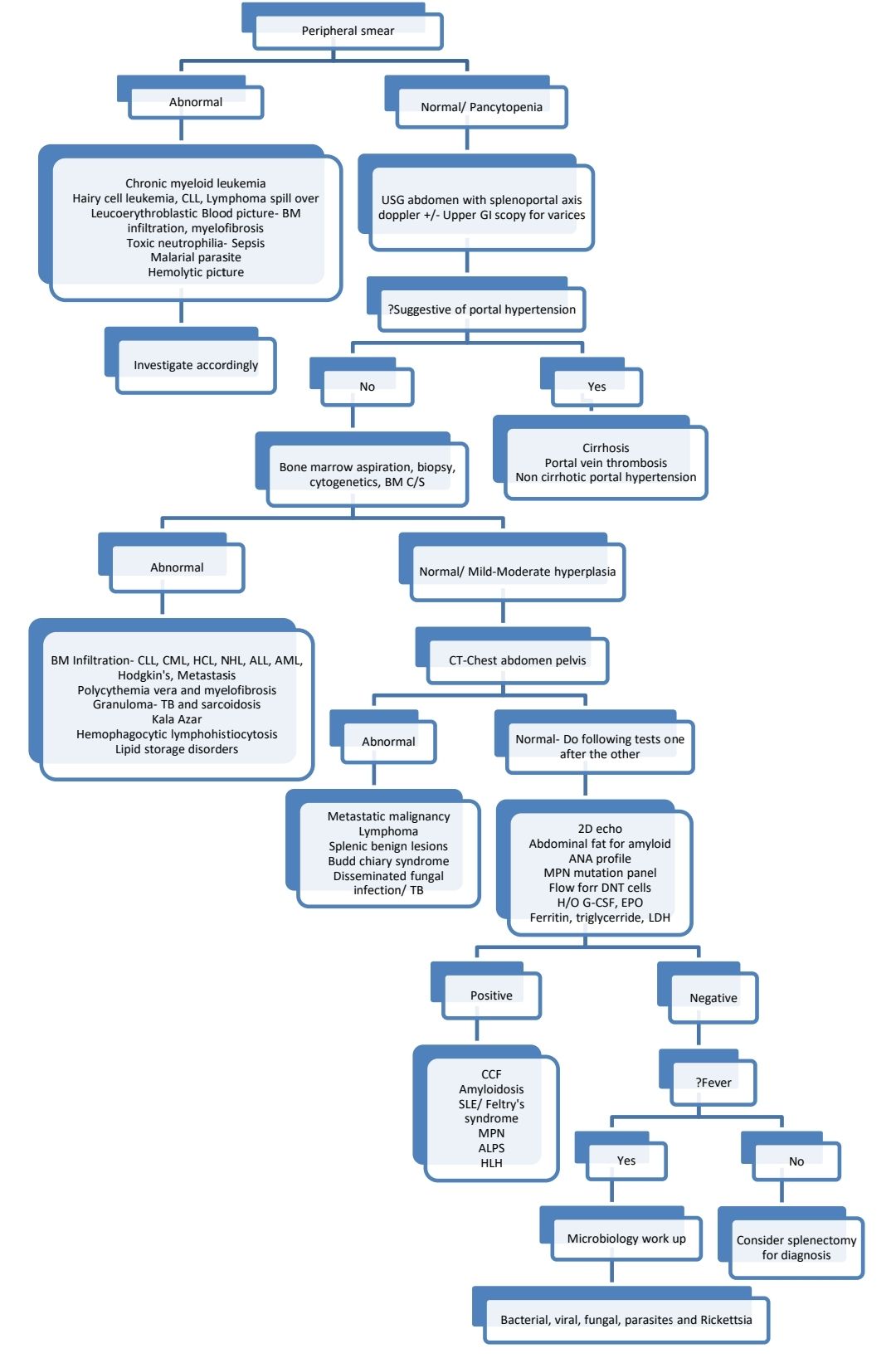
Diagnostic algorithm:
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.