howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Thrombocytosis
Introduction
- It is a condition in which platelet count is more than 4,50,000/cmm
- TPO is produced from liver and its level is inversely proportional to platelet count
Causes:
- Spurious
- Microspherocytes- Ex: Severe burns
- Cryoglobulinemia
- Neoplastic cell cytoplasmic fragments Ex- Acute leukemia
- Schistocytes
- Bacteria
- Pappenheimer bodies
- Clonal disorders:
- Essential thrombocythemia
- Polycythemia vera
- Primary myelofibrosis
- Myelodysplasia with del 5q
- Refractory anemia with ringed sideroblasts with marked thrombocytosis
- Chronic myeloid leukemia (They can have only thrombocytosis)
- Chronic myelomonocytic leukemia
- Atypical chronic myeloid leukemia
- MDS/MPN-U
- Hereditary essential thrombocytosis due to germline mutation of MPL- S505A mutation
- Inflammation associated
- Can be due to infections/ tissue damage
- It is cause of thrombocytosis in 80% of cases
- Thrombocytosis occurs due to release of IL6 and Interferon gamma
- ESR and CRP are increased
- Others
- Iron deficiency anemia
- Hyposplenism: Post splenectomy, functional asplenia (amyloidosis, celiac sprue)
- Post operative
- Post exercise
- Hemorrhage/ blood loss
- Malignancy including lymphomas
- Hemolysis
- Drug therapy: Corticosteroids, adrenaline, vincristine
- Cytokine administartion Ex: Thrombopoietin
- Rebound following myelosuppressive chemotherapy
- Acquired type II vWD
- Familial thrombocytosis due to mutations in TPO and TPO receptor genes
Clinical manifestations:
- Vasomotor symptoms: Headache, visual symptoms, light headedness, atypical chest pain, acral dysesthesia, erythromelalgia
- Thrombotic symptoms and bleeding- rarely seen with reactive thrombocytosis
- Splenomegaly- Often seen with ET
Investigations:
- CRP and ESR- Elevated in case of inflammatory status
- Iron profile
- Peripheral smear
- Microcytosis indicates iron deficiency anemia
- Leucoerythroblastic blood picture- Marrow infiltration/ fibrosis
- Acanthocytes, target cells- Seen after splenectomy
- Howell Jolly Bodies- Indicates hyposplenism
- Neutrophilia with shift to left- Seen in CML and infections
- Large poorly stained platelets- Seen in ET
- Tear drop cells- PMF
- Schistocytes/ circulating progenitor cells- Cause for false increase in platelet count
- Bone marrow aspiration and biopsy
- Secondary thrombocytosis
- Megakaryocytic hyperplasia with normal mature and left shifted megakaryocyte morphology
- Normal interstitial distribution and do not show clustering
- Reticulin- Not increased
- Essential thrombocytosis
- Normocellular/ mildly hypercellular
- Giant megakaryocytes with hyperlobated (staghorn) nuclei are seen
- Emperipolesis is often seen
- Small and also pyknotic megakaryocytes may be seen
- Normal erythropoiesis and granulopoiesis are seen
- No dysplasia is seen
- Iron stores are reduced
- Megakaryocytes are increased in number and are present as single cells or may form occasional small loose clusters within the interstitium
- Reticulin- 0-2+/4+
- Polycythemia vera
- Panmyelosis is seen
- Relatively increased erythroids
- Megakaryocytes are small and show marked pleomorphism with higher than normal nucleo cytoplasmic ratio
- Loose clustering of megakaryocytes is seen
- Storage iron is absent
- Primary myelofibrosis
- Megakaryocytes are markedly abnormal, with elongated and angulated shapes
- They are present adjacent to bony trabeculae and within sinuses
- Megakaryocytes may form dense and often large clusters
- High nucleocytoplasmic ratio is noted. Nuclei are enlarged, hyperchromatic and poorly lobulated
- MDS with 5q deletion
- Macrocytic RBCs with minimal polychromasia
- Normocellular bone marrow with dyserythropoiesis
- Increased megakaryocyes, present in the interstitium
- They are small and have monolobed/ hypolobated nuclei,that is eccentrically placed
- RARS with thrombocytosis
- Ringed sideroblasts seen
- CML
- Small hypolobulated megakaryocytes
- Secondary thrombocytosis
Morphological feature | ET | Pre-PMF |
Cellularity (age-adjusted) | Normal | Increased |
Myeloid-to-erythroid ratio | Normal | Increased |
Dense megakaryocyte clusters | Rare | Frequent |
Megakaryocyte size | Large/giant | Variable |
Megakaryocyte nuclear lobulation | Hyperlobulated | Bulbous / hypolobulated |
Reticulin fibrosis, grade 1 | Very rare | More frequent |
- Cytogenetics
- Abnormalities indicate clonal disorder
- JAK2 mutation testing
- Positive in 50% of ET and 97% of PV
- mpl mutation
- Seen in 10% of ET
- BCR-ABL mutation testing
- Presence is diagnostic of CML
- Should be done if there is basophilia or shift to left of neutrophils
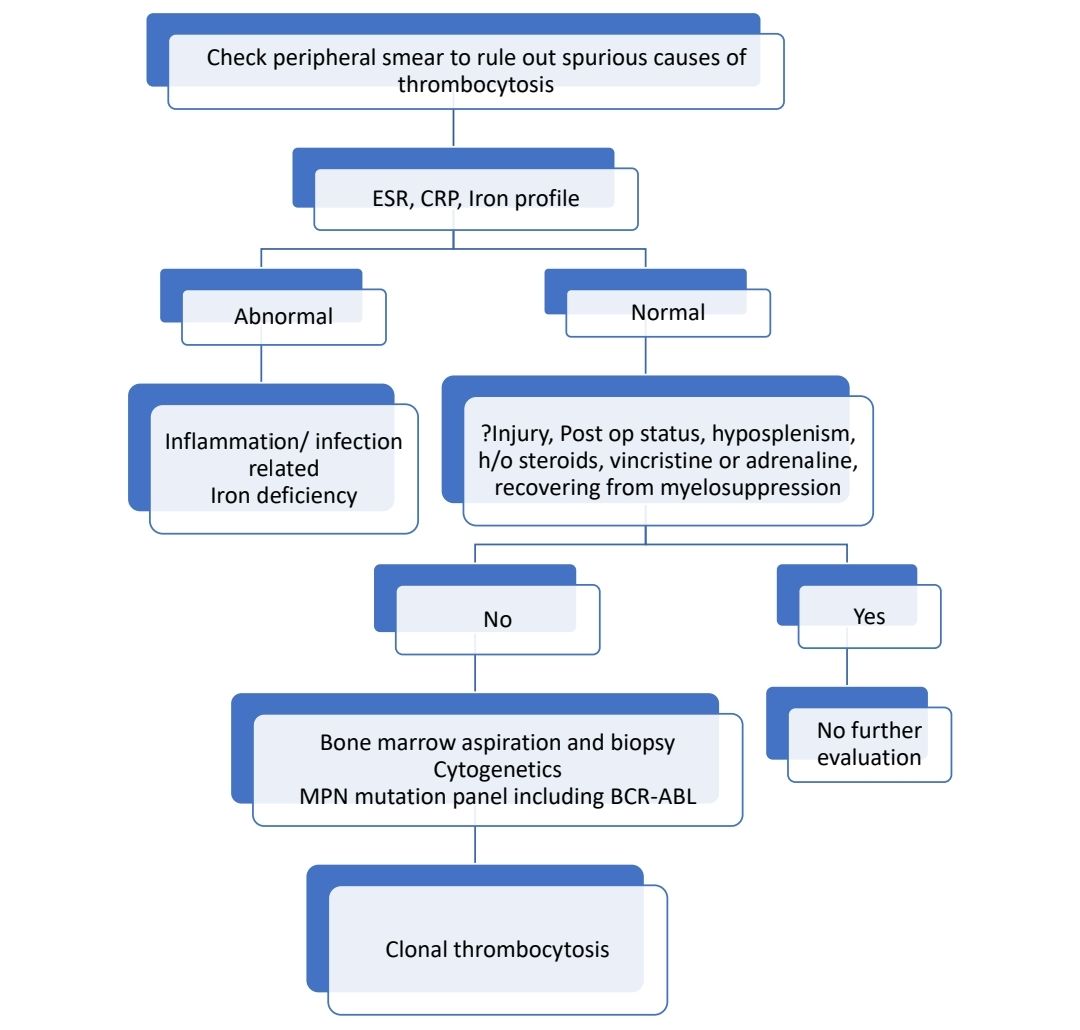
Diagnostic algorithm:
Treatment of reactive thrombocytosis:
- Resolves once underlying reactive state has been treated
- No data to support use of Aspirin
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.