howitreat.in
A user-friendly, frequently updated reference guide that aligns with international guidelines and protocols.
Eosinophilia and Basophilia
Updated on: 09.06.2025
Eosinophilia
Introduction:
- It is a condition in which absolute eosinophil count is more than 500/cmm
- Hypereosinophilia (HE): AEC >1500/cmm on at least 2 occasions over an interval of at least 4 weeks
- Hypereosinophilic syndrome (HES): Elevation of peripheral blood eosinophils (>1500/cmm) for more than 4 weeks associated with end organ damage. (“syndrome” applies to organ damage that can be attributed to the eosinophilic infiltrate)
- Cause of HE or HES can be:
- Secondary/ Reactive
- Primary/Clonal/Neoplastic
- Idiopathic/ Unexplained.
- Definition of Idiopathic hypereosinophilia (Hypereosinophilia of uncertain significance): It is unexplained AEC >1500/cmm on at least 2 occasions over an interval of at least 4 weeks, but there is no end organ damage.
- Difference between CEL-NOS and Idiopathic HES/HE is- CEL-NOS is a clonal disorder, i.e. cytogenetic abnormality is present or they have abnormal bone marrow morphology.
Causes:
- Primary:
- Myeloid/lymphoid neoplasms with eosinophilia and tyrosine kinase gene fusions ( PDGFRA, PDGFRB, FGFR1, JAK2, FLT3, ABL1, etc)
- MPN with eosinophilia (eg, CML and JAK2 V617F+ MPN)
- AML with inv(16) or t(16;16)/CBFB-MYH11
- MDS with eosinophilia
- MDS/MPN with eosinophilia
- Aggressive systemic mastocytosis with eosinophilia
- CEL-NOS
- Infections/ Infestations:
- Helminthic (Most common cause worldwide)-Ascaris (Loffler’s syndrome), toxocariaris, Loa loa, filariasis (tropical pulmonary eosinophilia), river blindness, Hook worm, strongyloides stercoralis, trichinella spiralis, other intestinal worms, oncocerciasis, schistosomiasis, fasciola, ecchynococcosis, toxoplasma, Paragonimus, Clonorchis
- Bacterial
- Mycobacterial
- Invasive fungal: coccidioides, histoplasma, cryptococcus, pneumocystis, aspergillosis
- Rickettsial
- Viral: HIV, HSV, HTLV-2
- Allergic conditions
- Allergic rhinitis
- Atopic dermatitis
- Allergic gastroenteritis
- Urticaria/ angioedema
- Asthma.
- Allergic bronchopulmonary aspergillosis (History of asthma, increased aspergillus specific IgE and IgG, IgE>1000ng/ml, wheal and flare skin reaction to aspergillus antigen, AEC- >1000/cmm)
- Drugs
- Antibiotics: penicillin, cephalosporins
- NSAIDS
- Antipsychotics
- Phenytoin
- Diet supplements
- Herbal remedies
- Aspirin
- GM-CSF therapy
- IL2 therapy for melanoma/RCC
- Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome: Occurs 3-6 weeks after introduction of new drug, Triad of skin eruptions, fever and internal organ involvement (Lung, liver, kidney, LN or heart)
- Connective tissue diseases
- Hypersensitivity vasculitis
- Churg Strauss syndrome
- Serum sickness
- Eosinophilic fasciitis (Schulman's disease)- Scleroderma like syndrome of unknown cause, Painful swelling and induration of limbs and trunk, increased gamma globulins, increased ESR and increased AEC.
- Sjorgen syndrome
- Rheumatoid arthritis
- Polyarteritis nodosa
- Systemic lupus erythematosus
- Inflammatory bowel disease
- Celiac disease
- Sarcoidosis
- Systemic sclerosis
- IgG4-related disease
- Neoplasms
- Internal malignancies- Ex: renal, lung, breast, vascular neoplasms, female genital tract cancers
- Hematological malignancies- Hodgkin and Non-Hodgkin lymphoma, Langerhan's cell histiocytosis
- GI disorders
- Eosinophilic gastroenteritis
- Eosinophilic esophagitis
- Celiac disease
- Inflammatory bowel disease
- Allergic gastroenteritis
- Chronic pancreatitis
- Respiratory disorders.
- Pulmonary eosinophilia (Loeffler syndrome)- Transient pulmonary reaction with reticulo-nodular shadowing on CXR associated with peripheral blood eosinophilia, Low grade fever and cough for 7-10 days, Usually due to allergic reaction to parasites/drugs, Self limiting within 3-4 weeks of eliminating causal agent.
- Bronchiectasis, cystic fibrosis
- Hypersensitivity pneumonitis
- Eosinophilic pneumonia (At least 25% eosinophils in alveolar eaves)
- Cardiac disorders:
- Tropical endocardial fibrosis
- Eosinophilic endomyocardial fibrosis or myocarditis
- Skin diseases.
- Atopic dermatitis
- Eczema
- Scabies
- Myiasis
- Scarlet fever
- Bullous pemphigoid
- Eosinophilic cellulitis (Well syndrome)- Sudden onset of annular/ circinate erythematous edematous patches that rapidly evolve to morphea like slate blue plaques
- Recurring granulomatous dermatitis
- Dermatitis herpetiformis
- Herpes gestationalis
- Gleich syndrome (Variant of hypereosinophilic syndrome, recurrent episodes of angioedema, usually monthly intervals, sometimes associated with eosinophilic cellulitis, resolves spontaneously without therapy, corticosteroids decrease the severity of attack)
- Inherited disorders:
- Wiskott aldrich syndrome
- Severe combined immunodeficiency (Swiss type/ X linked)
- Selective IgA deficiency with atopy
- Nezelof syndrome
- Hyper IgE syndrome (Job's syndrome)
- Familial hypereosinophilia: Autosomal dominant, beigins at birth, usually do not have eosinophilic activation, occurs due to dysregulation of IL-5 mRNA expression
- DOCK 8 deficiency
- PGM3 deficiency
- Miscellaneous:
- Eosinophilia-Myalgia syndrome
- Toxic oil syndrome (Cooking oil contaminated with tryptophan)
- Cholesterol athero-embolic disease with catheterization procedure
- GVHD- Both acute and chronic
- Solid organ rejection
- Adrenal insufficiency
- Benign eosinophilia (Increased eosinophils with no symptoms or organ damage)
- Angiolymphoid hyperplasia with eosinophilia (Kimura disease)
- Lymphocytic variant of HES: Expansion of phenotypically aberant T lymphoid cells (eg, CD3+/CD4−/CD8− or CD3−/CD4+) with reactive eosinophilia, without overt lymphoproliferative disorder. Typically have cutaneous manifestations. Treated same as idiopathic HES.
Grading of eosinophilia:
- Mild- Up to 1000/cmm
- Moderate- 1000-5000/cmm
- High- >5000/cmm
Pathogenesis:
IL-5, IL-3, or granulocyte-macrophage colony-stimulating factor from activated T cells/ Mast cells/ stromal cells/ tumor cells
or
Tyrosine kinase gene fusions
↓
Increased proliferation of eosinophils which may subsequently infiltrate tissues
↓
Release of mediators such as eosinophil-derived cationic protein, major basic protein 1and 2, peroxidase, and neurotoxin
↓
Local inflammation, tissue remodeling, and sometimes tissue damage
↓
Tissue fibrosis and/or thrombosis with end-organ damage
Clinical features in hypereosinophilic syndrome:
- Skin (40%–70%): Pruritus, papule / plaques, angioedema, mucosal ulcers, vesciculo-bullous lesions
- Lungs (25%–40%): Pulmonary infiltrates, fibrosis, pleural effusion and pulmonary embolism
- Gastrointestinal tract (15%–35%): Diarrhoea, ascites, gastritis, colitis, pancreatitis, cholangitis, hepatitis, Budd chiary syndrome
- Heart (5%–20%) : Myocardial infarction, acute heart failure, thromboembolism, endomyocardial fibrosis, restrictive cardiomyopathy, Pericarditis, myocarditis, intramural thrombus formation, scarring of mitral / tricuspid valves leading to regurgitation
- Nervous system (5%–20%): Peripheral neuropathy, mononeuritis multiplex, paraparesis, cerebellar dysfunction, epilepsy, dementia, cerebrovascular accident, eosinophilic meningitis, encephalopathy, dementia
- Others- Microthrombi, vasculitis, retinal arteritis, digital necrosis, muscle pain, arthritis, arthralgia, Raynaud's phenomenon
Investigations: (Done based on initial evaluation and degree of clinical urgency)
- Full blood count with peripheral smear- For blasts/ parasites
- RFT
- LFT
- LDH
- Uric acid
- ESR and CRP- To rule out inflammatory/ reactive disease
- Vitamin B12- Increased in case of myeloid disorders
- Stool for ova and cyst
- Serology for strongyloides, schistosomiasis, filariasis, toxocara
- S. IgE levels
- Quantitative immunoglobulin levels
- Flow cytometry for T abd B subset analysis
- BCR-ABL and PDGFR mutations
- BM aspiration and biopsy
- Done if there is no identifiable cause and BCR-ABL and PDGFR mutations are negative.
- Same time perform cytogenetics and flow for CLPD
- Chest X ray and spirometry
- CT Chest and 2D Echo- for noting end organ damage. These should be done along with the tests done for cause of eosinophilia
- S. Tryptase- For systemic mastocytosis
- S. Cortisol
- S. IL5 levels
- GI biopsy
- HIV and HTLV serology- In patients with suspected opportunistic infections
- Flow cytometry for aberrant T-cell immunophenotype
- Investigations related suspected cause such as ANA, ANCA, bronchoscopy, imaging etc
- NGS myeloid panel: Should be done if the karyotype is normal or of no diagnostic significance (eg, loss of Y chromosome in elders)
Compared to other hyper-eosinophilia patients with clonal/ neoplastic eosinophilia have:
- Constitutional symptoms, such as fever, weight loss, fatigue, cough, dyspnea etc
- Splenomegaly and/ or lymphadenopathy
- Peripheral blood: Presence of both mature and immature and/or dysplastic cells; anemia; abnormal platelet count (thrombocytopenia or thrombocytosis)
- Abnormal morphology in bone marrow: Increased blasts, dysplasia and bone marrow fibrosis
- Immunophenotypic aberrancy in the blast population
- Abnormal T cell population
- Patients are older
- High leucocyte count with high percentage of eosinophils and neutrophilia, monocytosis and/or basophilia
- Elevated S. Tryptase levels (>12 ng/mL)
- Increased Vitamin B12 levels (>1000 pg/mL)
- Eosinophilia that is refractory to steroids
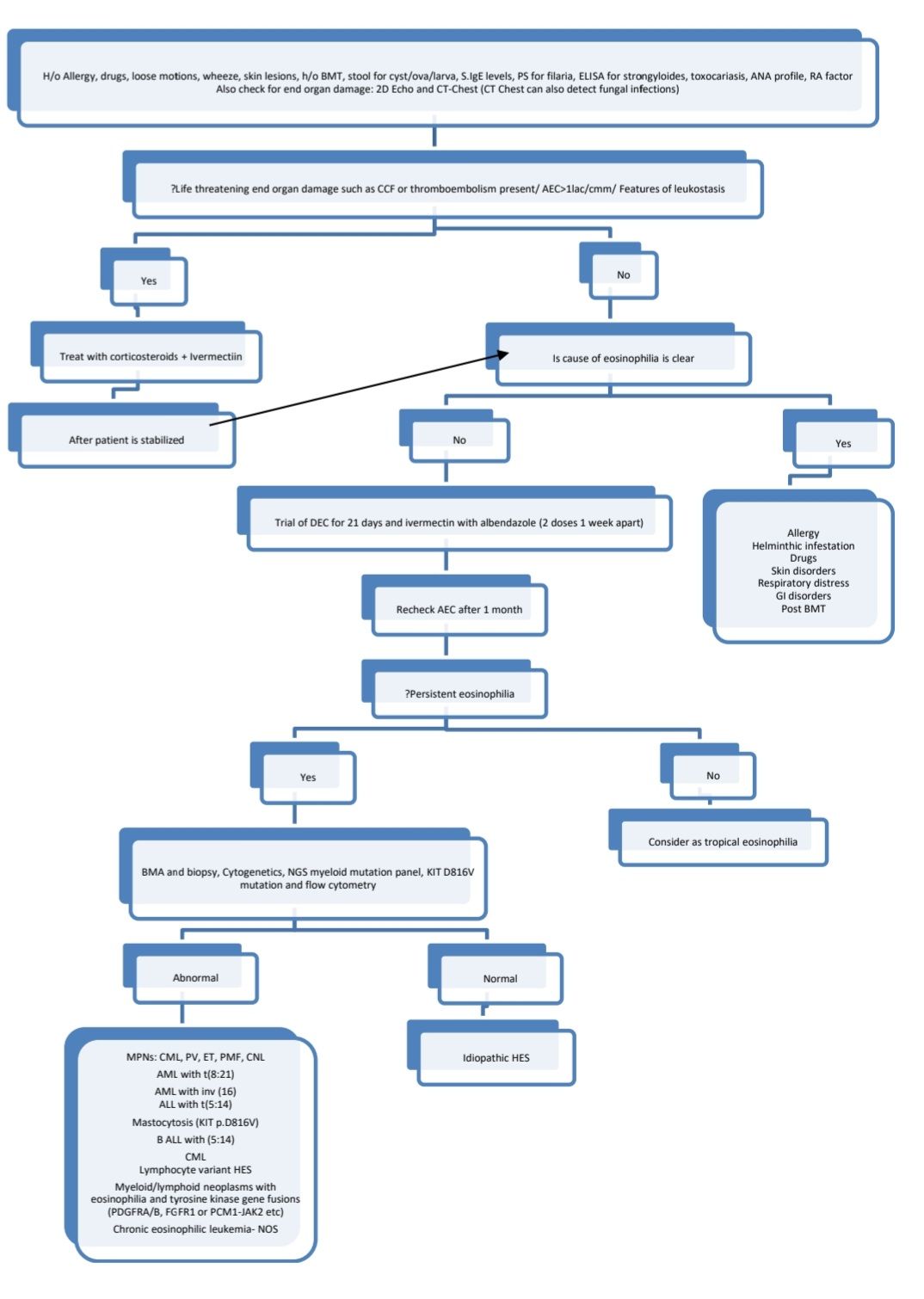
Diagnostic algorithm:
Idiopathic hypereosinophilic syndrome:
- It has following characteristics
- Unexplained elevation of peripheral blood eosinophils (>1500/cmm) for more than 6 months
- No reactive causes of eosinophilia (Infections, allergy, autoimmunity, pulmonary conditions and neoplastic disorders)
- No associated clonal myeloid neoplasms such as AML, MDS, MPN or systemic mastocytosis
- No cytokine producing immunophenotypically aberrant T cell population
- No increased myeloblast in the peripheral blood or bone marrow
- No evidence of clonality
- Associated end organ damage
- Definition of Idiopathic hypereosinophilia/ Hypereosinophilia of unknown significance: It is same as above, but there is no end organ damage
- If clonality is established (by cytogenetics/ PCR/ NGS for myeloid malignancies/High blast count- >2% in PB and >5% in BM), then such case are redefined as CEL-NOS.
Treatment of eosinophilia in general:
- Treatment of underlying cause in case of secondary eosinophilia
- For primary/ clonal eosinophilia- Refer section on Chronic Eosinophilic Leukemia
- Steroids and hydroxyurea, to reduce eosinophil counts rapidly and to reduce end organ damage
- In endemic areas use of broad spectrum antihelminthics is justified
- Emergency treatment (For patients with severe eosinophilia with end organ damage/ life threatening eosinophilia- AEC>1lac/cmm/ Features of leukostasis)
- High dose corticosteroids- Methyl prednisolone- 1mg/kg/day/ Oral prednisolone- 0.5mg- 1mg/kg/day for 2 weeks, then taper over 2-3 months to lowest possible dose to maintain response
- Give concomitant Ivermectin, if there is suspicion of strongyloides (200microgm/kg/day for 2 days)
- Treatment of idiopathic hypereosinophilic syndrome
- 1st line- Steroids (Prednisolone 0.5-1mg/kg/day) for 2 weeks, then slowly taper over 2-3 months to a lowest possible dose to maintain a response. Ivermectin cover (200microgm/kg- OD for 2 days) has to be given initially
- 2nd line (If there is inadequate response to steroids/ if there is need for prolonged steroid therapy/ intolerance to steroids) Short trial (4-6 weeks of following may be tried
- Imatinib- 400mg- OD- May be useful in patients without PDGFR mutation
- Interferon alpha- 1-5 million units/m2/day for initial few doses, then lower the doses as maintenance
- Azathioprine- 1-3mg/kg/day- Adjust the doses based on the response
- Ciclosporine- 150-300mg/day
- Hydroxyurea- 500-3000mg/day
- Cyclophosphamide
- Targeted therapies:
- Mepolizumab and Reslizumab- Anti-IL5 antibody
- Benralizumab- Binds to alfa chain of IL-5 receptor and induces eosinophil death via antibody dependent cell cytotoxicity (throgh NK Cell)
- Lirentelimab- Antibody to Singlec8 that depletes eosinophils and inhibits mast cell activation
- Dupilumab- Monoclonal antibody to IL4 receptor alfa. Approved for treatment of eosinophilic esophagitis
- Dexpramipexole: Causes maturation arrest and eosinophilic depletion through an unknown mechanism
- 3rd line (If not responding to any of the 2nd line agents)
- Alemtuzumab
- Hematopoietic stem cell transplantation
Basophilia
- It is a condition in which absolute basophil count is more than 100/cmm
- Causes
- Allergy or inflammation (Associated with increased IgE)-
- Ulcerative colitis
- Drug, food, inhalant hypersensitivity
- Erythroderma, urticaria
- Juvenile rheumatoid arthritis.
- Endocrinopathy
- Diabetes mellitus
- Estrogen administration
- Hypothyroidism
- Infections
- Chicken pox
- Influenza
- Tuberculosis
- Iron deficiency
- Exposure to ionizing radiations
- Neoplasia
- MPN- CML, PV, PMF, ET
- AML with t (9:22) and t(3:6) or 12p abnormalities
- AML with basophilic maturation
- Carcinoma
- Allergy or inflammation (Associated with increased IgE)-
An Initiative of
Veenadhare Edutech Private Limited
1299, 2nd Floor, Shanta Nivas,
Beside Hotel Swan Inn, Off J.M.Road, Shivajinagar
Pune - 411005
Maharashtra – India
howitreat.in
CIN: U85190PN2022PTC210569
Email: admin@howitreat.in
Disclaimer: Information provided on this website is only for medical education purposes and not intended as medical advice. Although authors have made every effort to provide up-to-date information, the recommendations should not be considered standard of care. Responsibility for patient care resides with the doctors on the basis of their professional license, experience, and knowledge of the individual patient. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse effects, please refer to the approved product label. Neither the authors nor publisher shall be liable or responsible for any loss or adverse effects allegedly arising from any information or suggestion on this website. This website is written for use of healthcare professionals only; hence person other than healthcare workers is advised to refrain from reading the content of this website.